demyelination
evidence of demyelination, either through nerve conduction studies showing decreased peripheral nerve conduction velocity or peripheral nerve biopsy showing histologic evidence of segmental demyelination
demyelination
evidence of demyelination, either through nerve conduction studies showing decreased peripheral nerve conduction velocity or peripheral nerve biopsy showing histologic evidence of segmental demyelination
CIDP
In contrast to many other polyneuropathies (eg, diabetic), CIDP is not length dependent. Therefore, it classically causes both proximal (eg, hip girdle) and distal (eg, hand) muscle weakness.
Motor symptoms predominate, but distal sensory loss (eg, in the toes) can also occur; vibration and position sense are often preferentially affected due to greater involvement of large, thickly myelinated fibers. In addition, because CIDP involves peripheral nerves, lower motor neuron signs (eg, hyporeflexia, atrophy) may be seen.
sinus of Valsalva

headaches caused by cervical degenerative joint disease
Cervicogenic headaches are headaches which result from spinal problems in the neck, such as disc degeneration or prolapse, or facet joint arthritis. 'Cervico-' means neck, and '-genic' means origin. Cervicogenic headaches are quite common and under-recognised.
Secondary changes in the skin
If we use the CEAP classification, chronic venous disease includes all stages (C0-C6) and chronic venous insufficiency only includes C3-C6.
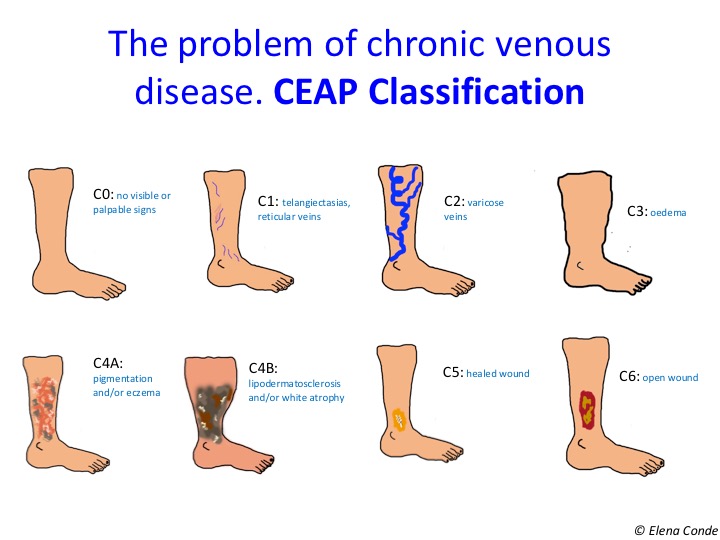

In fact, eczema secondary to venous hypertension and lipodermatosclerosis are the characteristic findings of stages C4a and C4b, respectively.

(brawny) skin hyperpigmentation
 Hyperpigmentation in the “gaiter area” due to chronic venous insufficiency.
Hyperpigmentation in the “gaiter area” due to chronic venous insufficiency.
liquefactive necrosis


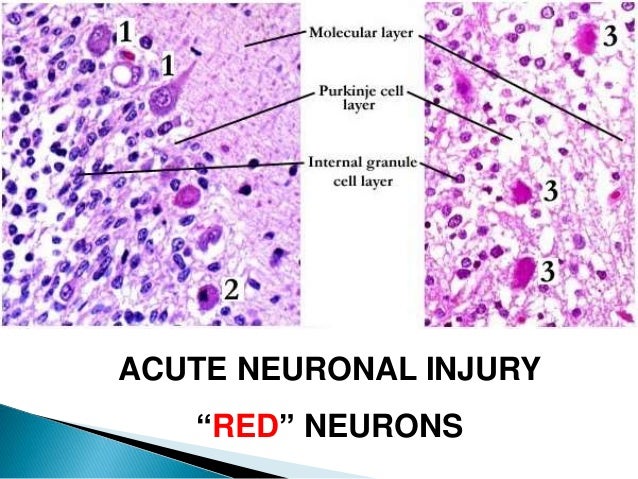
red neurons
karyorrhexis


parathyroid ADENOMAS

metastatic calcification of the renal tubules

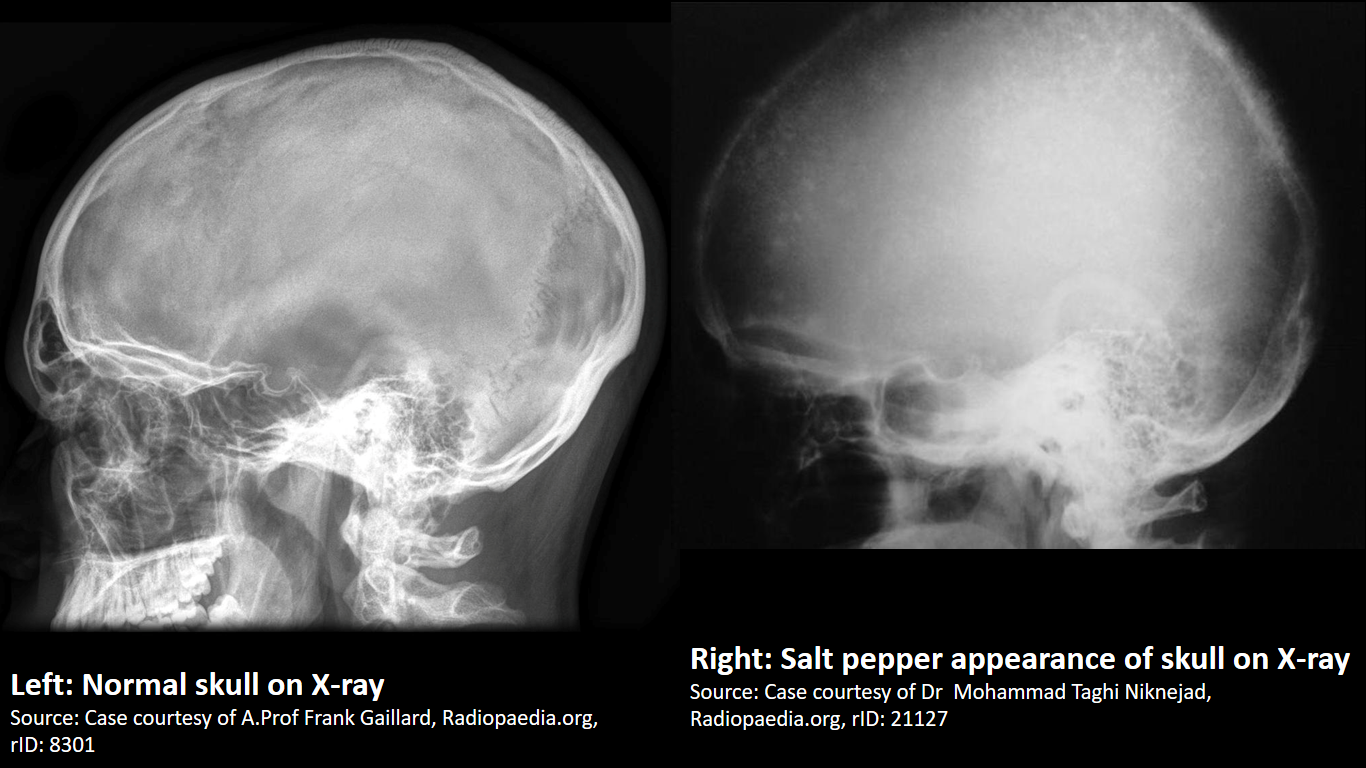
“salt and pepper” appearance of the skull
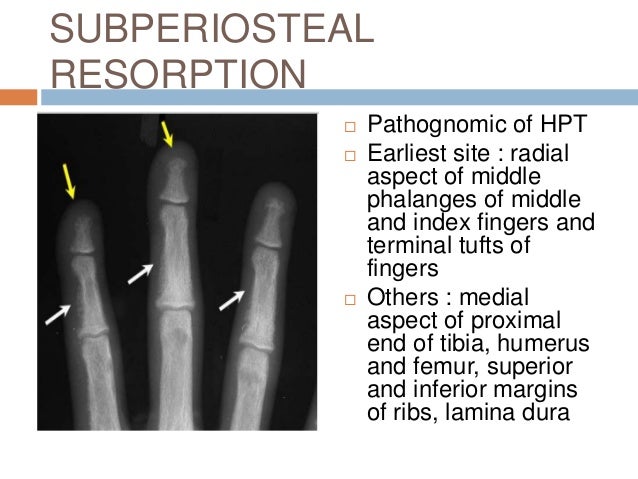
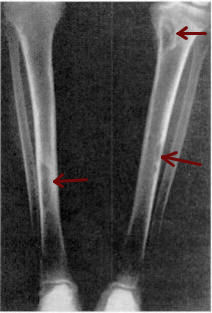
SUBperiosteal thinning of the phalanges
OSTEITIS FIBROSA CYSTICA

Thorotrast

angiosarcoma

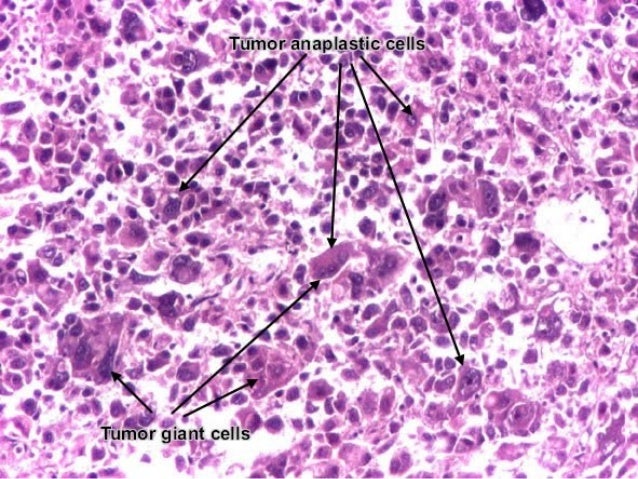
HCC contain “giant cells”
well-differentiated (“organized”) HCC tumors have bile-containing pseudo-canaliculi on histology

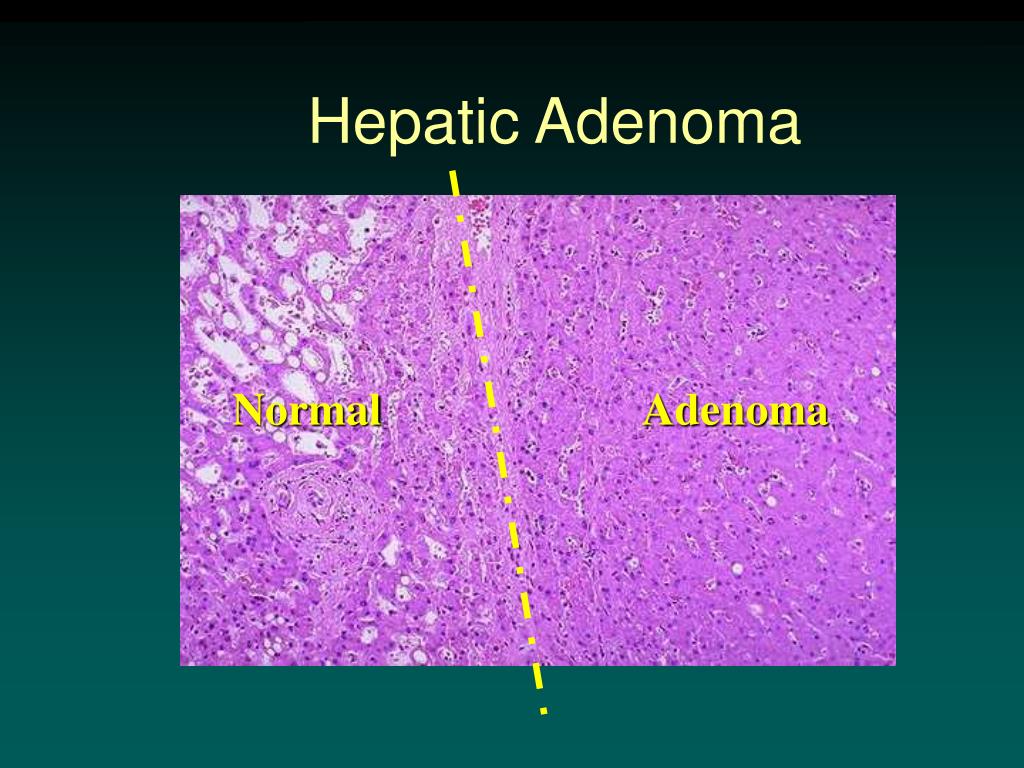
hepatic adenomas contain thin-walled vessels and sinusoids WITHOUT bile ducts

, hepatic adenomas are composed of large hepatocytes full of glycogen
“cavernous” dilated cystic areas
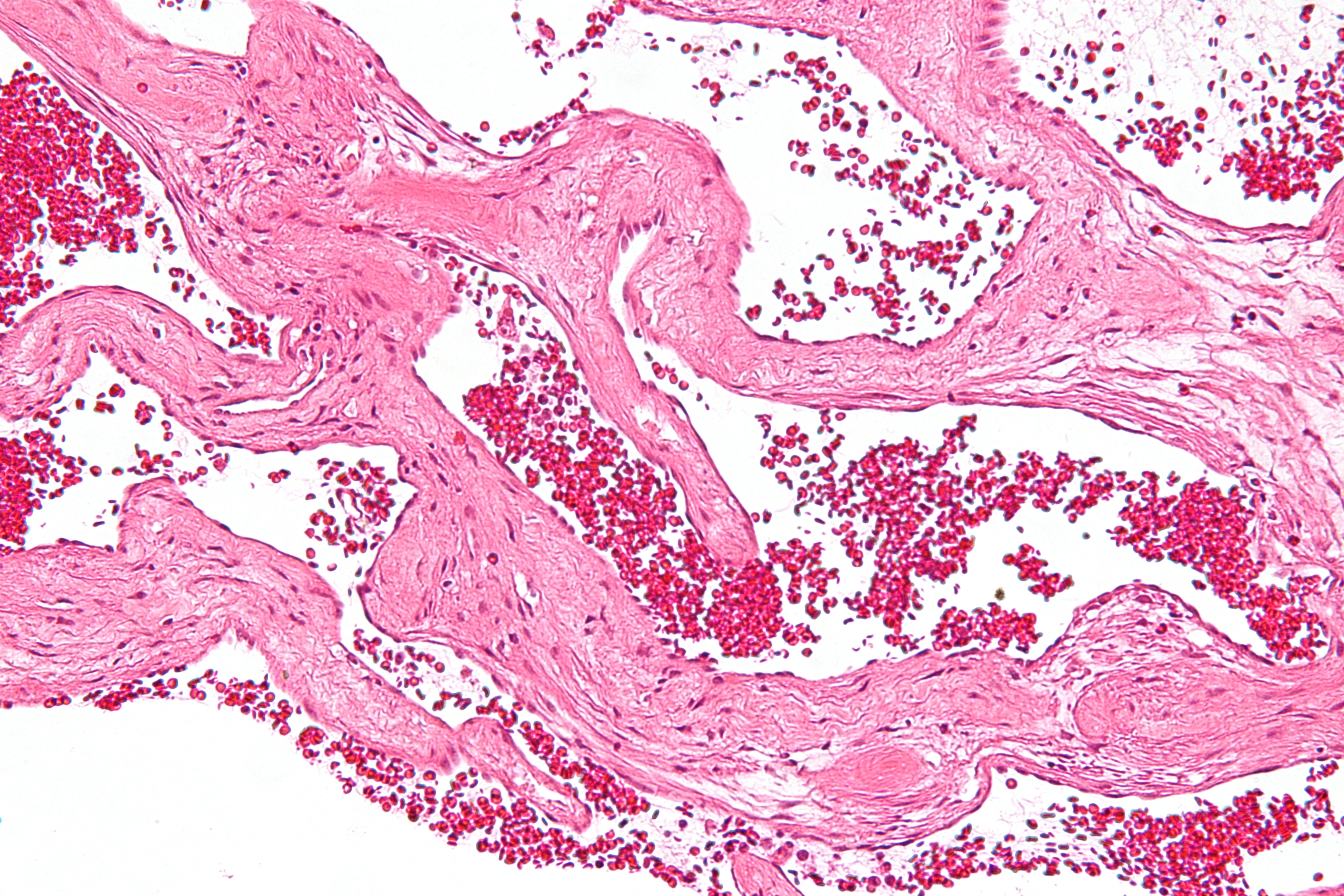
hepatic hemangioma
FNH has a large central artery

nodular star pattern
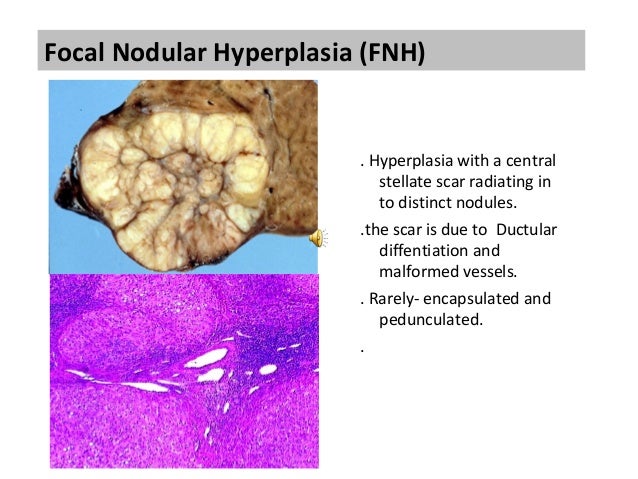
Focal Nodular Hyperplasia (FNH)
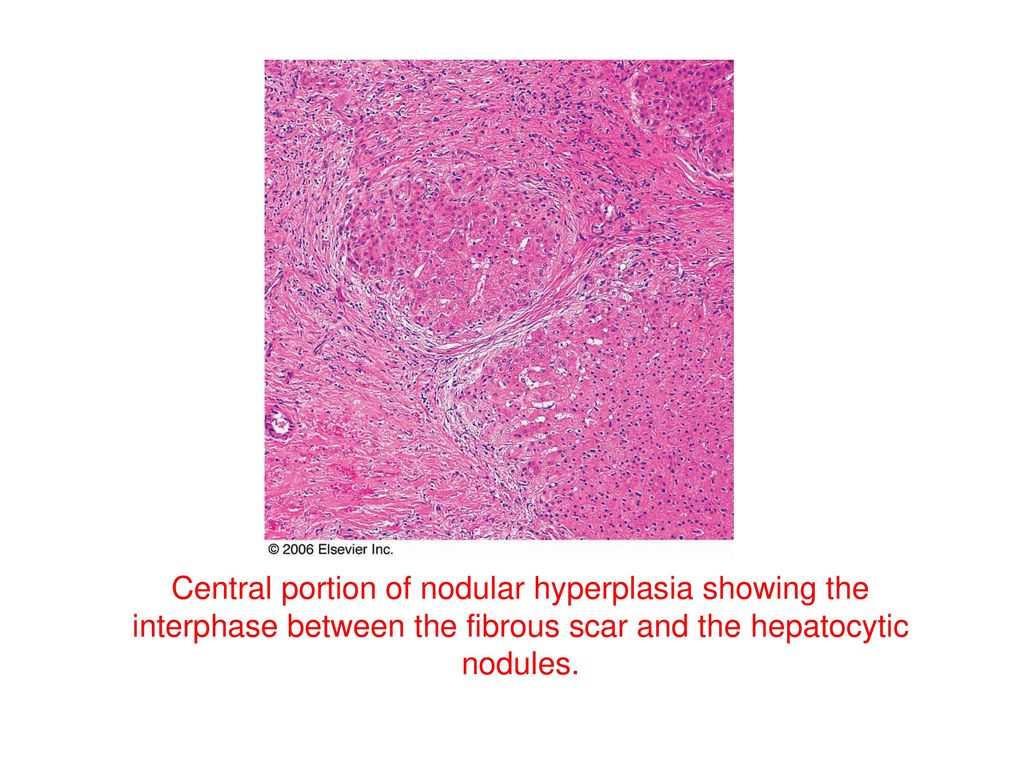
Focal Nodular Hyperplasia
INTESTINAL GANGLIONEUROMATOSIS
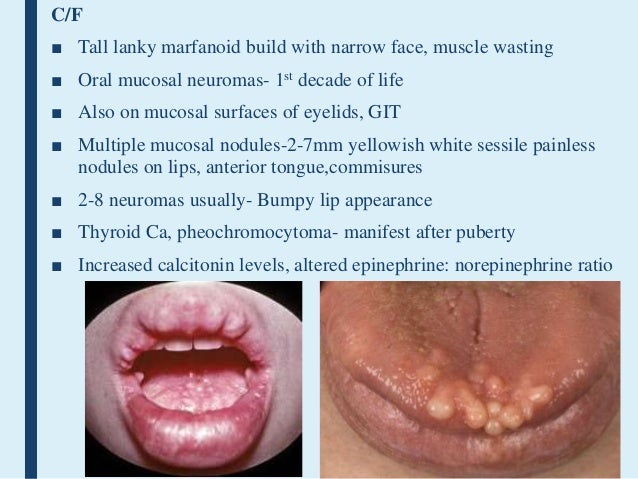
MUCOSAL NEUROMAS
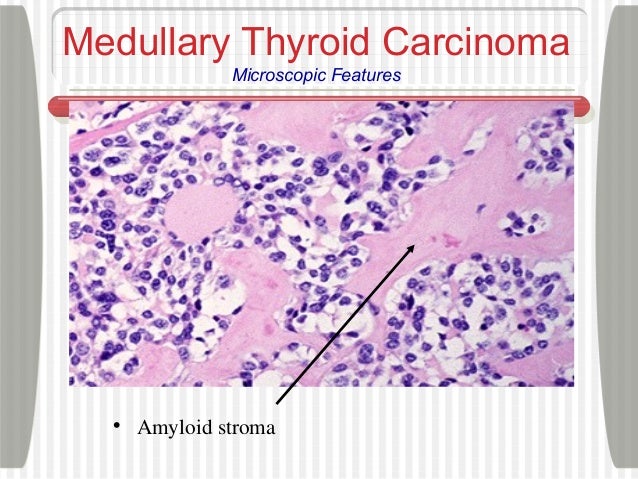
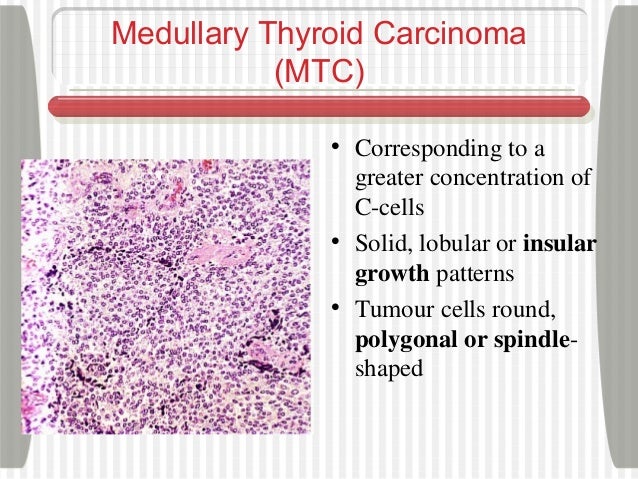
medullary thyroid carcinomas

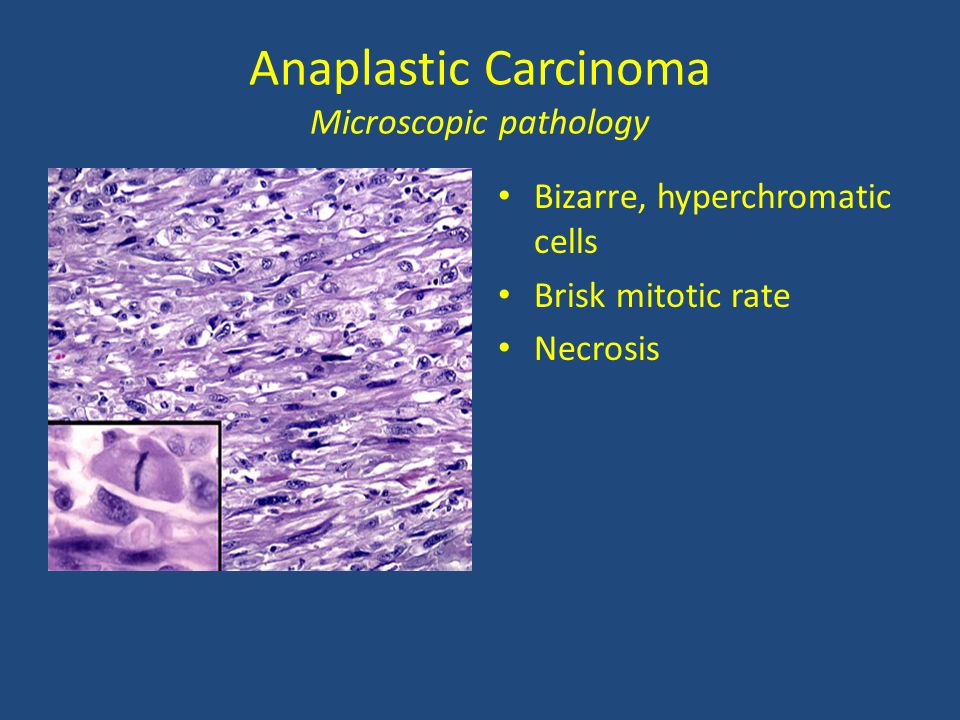
anaplastic thyroid carcinoma
follicular thyroid carcinoma
papillary thyroid carcinoma

follicular cells surrounding colloid
follicular adenomas
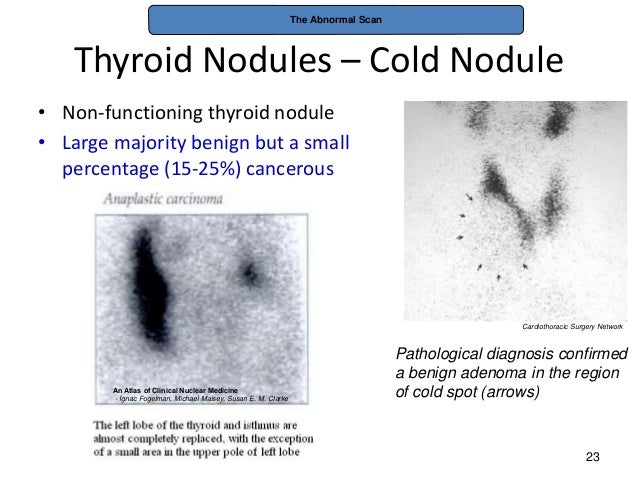
“cold” nodules
A cold nodule is a thyroid nodule that does not produce thyroid hormone. On a radioactive iodine uptake test a cold nodule takes up less radioactive material than the surrounding thyroid tissue. A cold nodule may be malignant or benign.
“hot” nodule radioactive iodine uptake
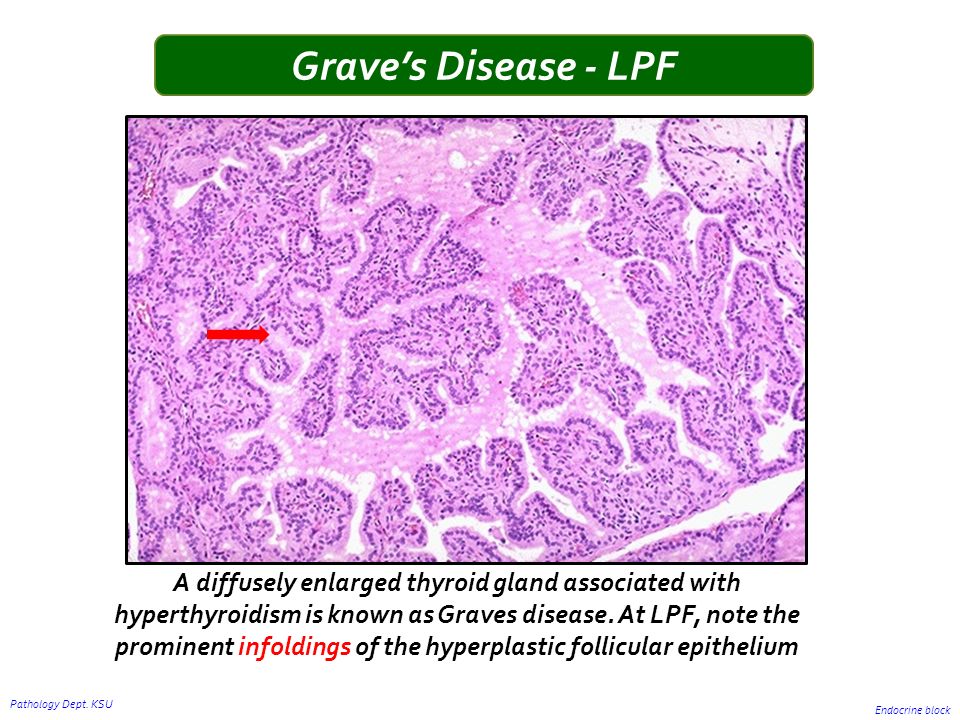
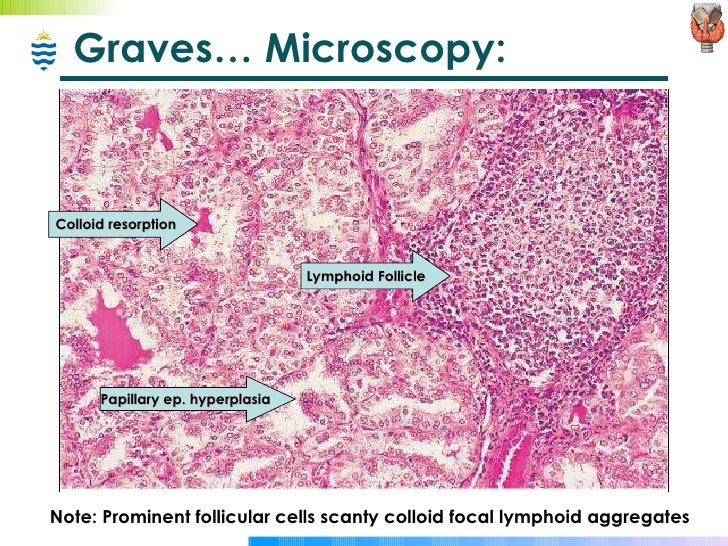
“scalloped” appearance of colloid

histologically, thyroid tissue in Graves’ disease

pretibial myxedema

thyroid storm

histologically, Riedel’s thyroiditis

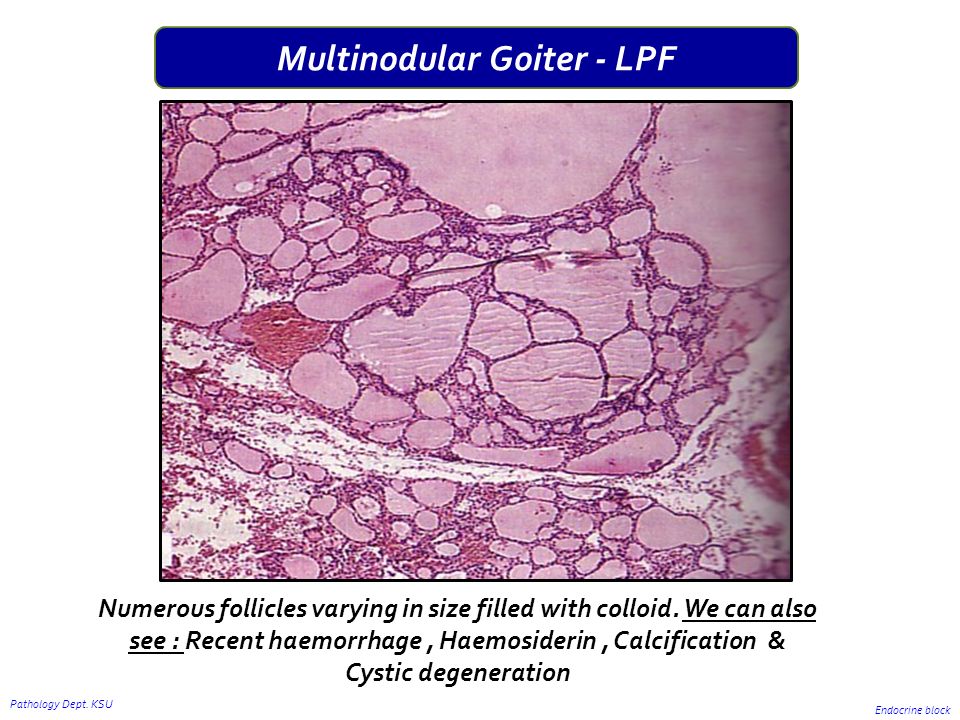
multinodular goiter
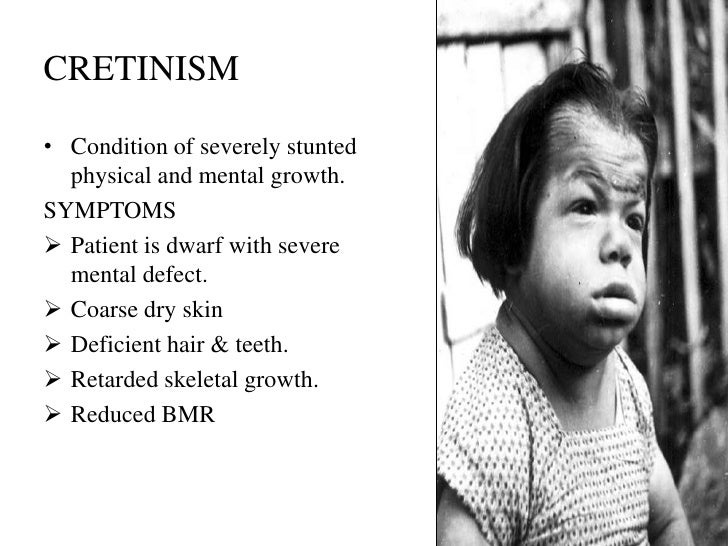
cretinism

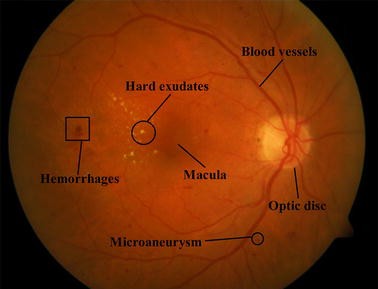
nonproliferative diabetic RETINOPATHY

necrobiosis lipoidica


Zellballen

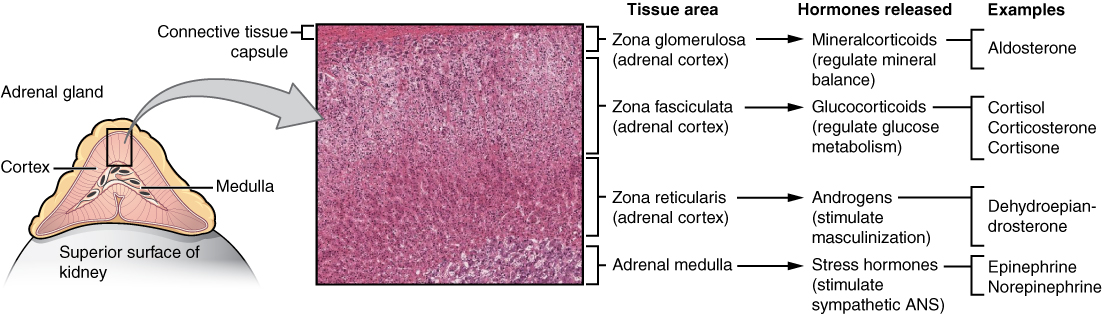
glucocorticoids

SPIRONOLACTONE bodies


chinese character-like appearance. It characteristically does not have osteoblastic rimming fibrous dysplasia affecting more than one bone
When polyostotic fibrous dysplasia manifests in the long bones, limping results; when it manifests in the face, asymmetric growth of the face can result
posterior urethral valve
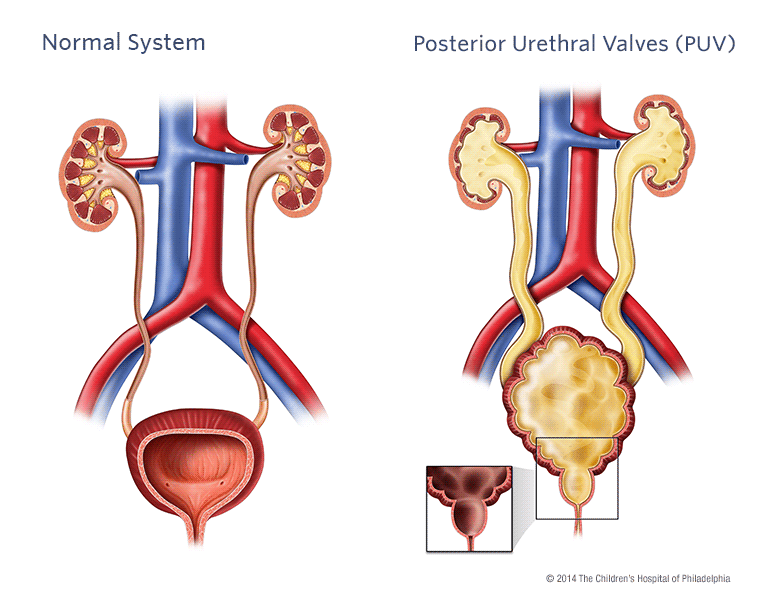

vesicoureteral reflux
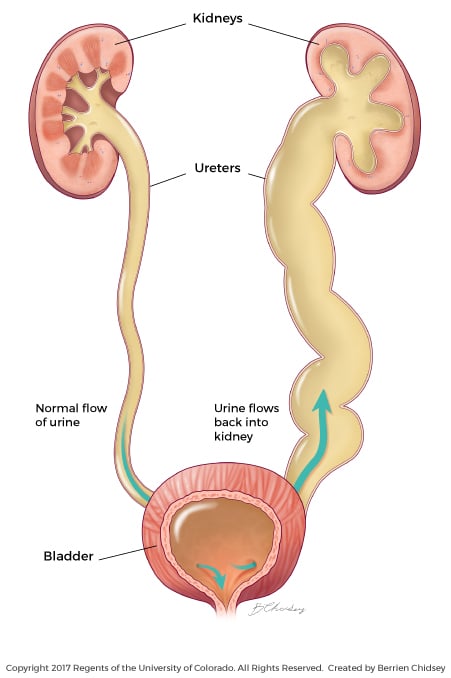
ureteropelvic junction obstruction

osteitis fibrosa cystica
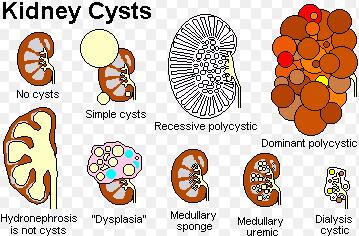
medullary sponge kidney
cystic disorders of the kidney
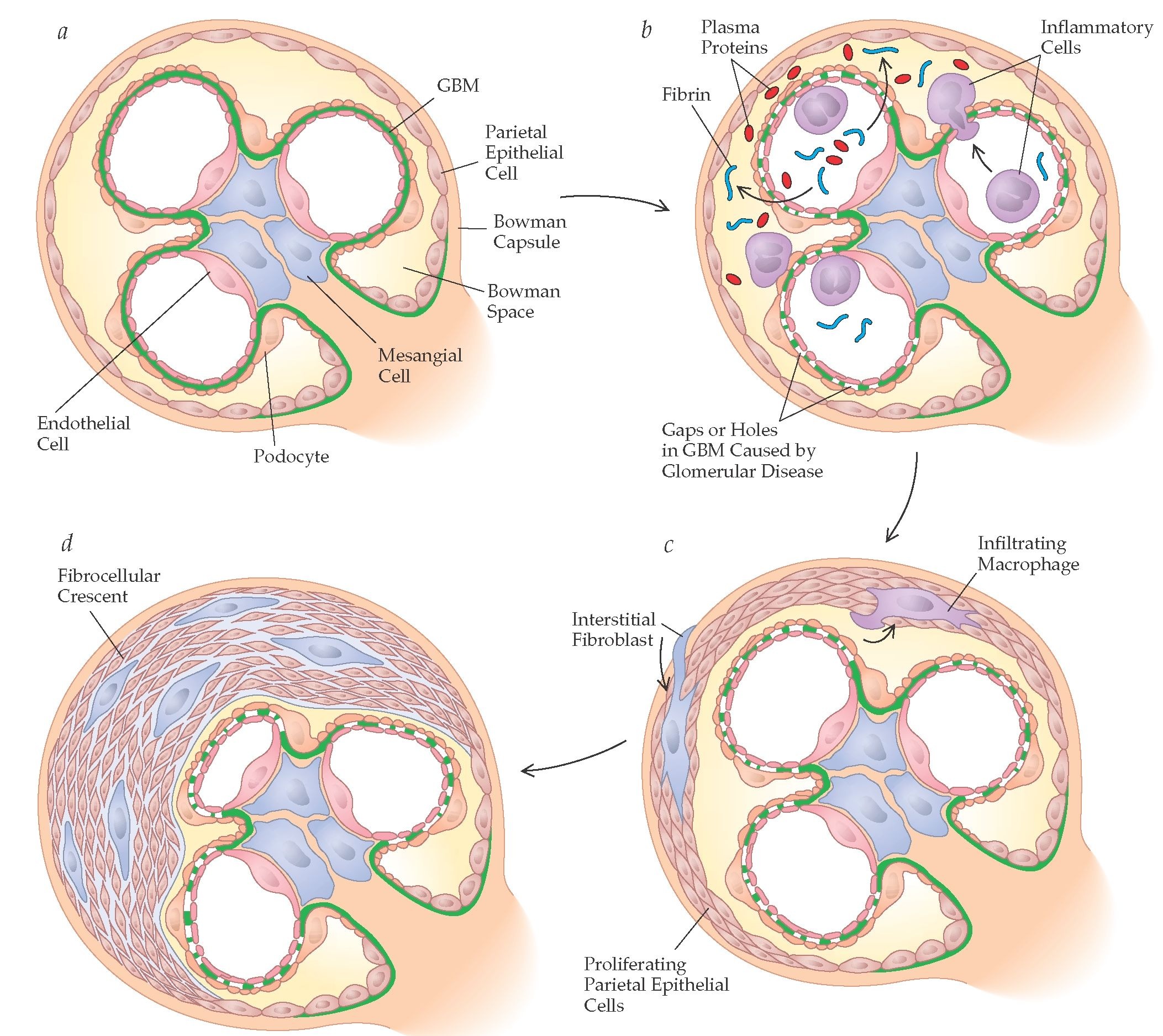
proliferation from the capsule (parietal)
anion gap
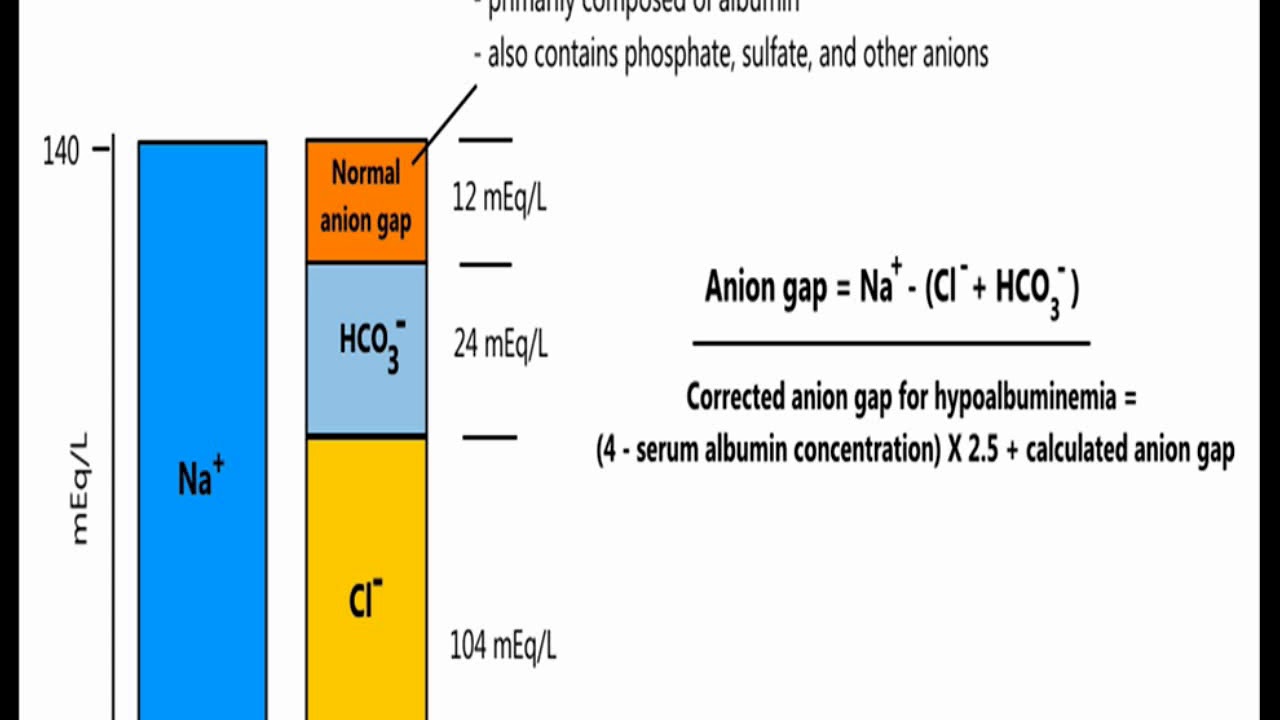
MUDPILES

metabolic syndrome

SESSILE SERRATED polyp

Proposed serrated pathway to colorectal cancer. Normal colonic crypts have regular test tube-like crypts with a smooth lumen. Hyperplastic polyps (HPs) have serrations in the upper two thirds of the crypt. In SSPs, serrations extend deeper into the crypt and the crypt base is often dilated and may have a boot or inverted BT^ shape. SSPs with cytologic dysplasia (SSP/Dys) have focal areas of conventional dysplasia (arrows) that are thought to rapidly progress to sporadic MSI-H CRCs.
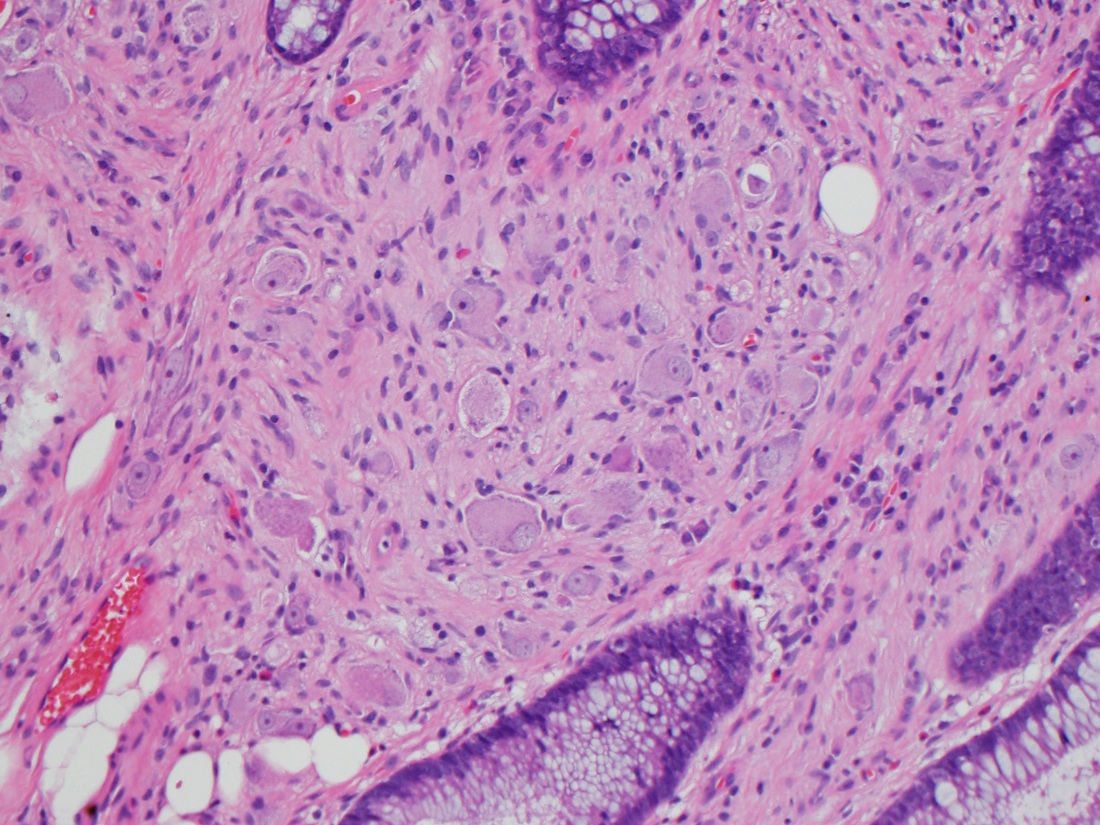
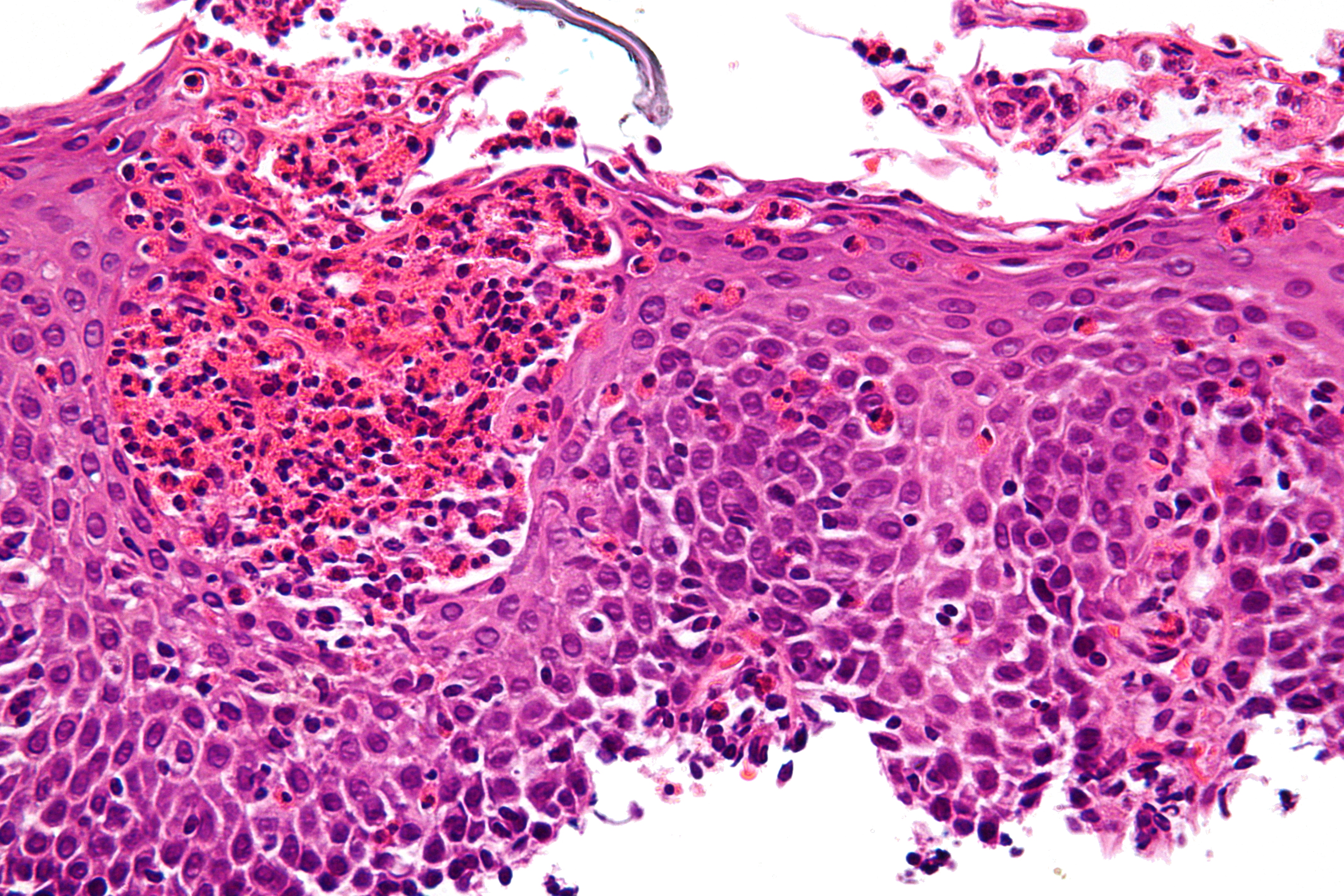
squamous cell carcinoma
Risk factors for anal cancer
Infection with human papillomavirus (HPV)
Condyloma acuminata
Chronic fistulas
Irradiated anal skin
Leukoplakia
Lymphogranuloma venereum
squamous cell carcinoma
Squamous cell carcinoma of the anorectum accounts for 3 to 5% of distal large-bowel cancers.
Metastasis occurs along the lymphatics of the rectum and into the inguinal lymph nodes.
colorectal cancer
Goal of cureResection of the primary colonic or rectal cancer Regional lymph node removal to determine staging For metastatic disease, resection of isolated liver or lung metastases
Goal of palliationFor unresectable rectal cancer, diverting colostomy or placement of an expandable wire stent
STAGE II DISEASE (more LOCALLY invasive tumor) Adjuvant chemotherapy beneficial for persons at high risk for recurrence (determined, in part, by CEA level)
STAGE III DISEASE (NODES INVOLVED) Adjuvant chemotherapy FOLFOX (oxaliplatin, fluorouracil, and leucovorin) is the preferred adjuvant therapy for most patients with stage III disease
STAGE IV (METASTATIC SPREAD) FOLFOX Possibly biologics
anal cancer
Rectal tenesmus Urgency Recurrent hematochezia
RIGHT-sided colon cancer
Iron deficiency anemia Fatigue Weakness from chronic blood loss
LEFT-sided colon cancer
Obstructive symptoms Colicky abdominal pain Change in bowel habits Constipation alternating with loose stools Stool streaked with blood
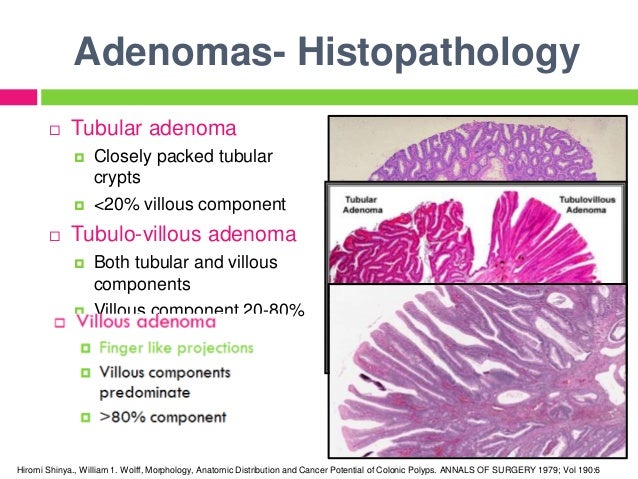
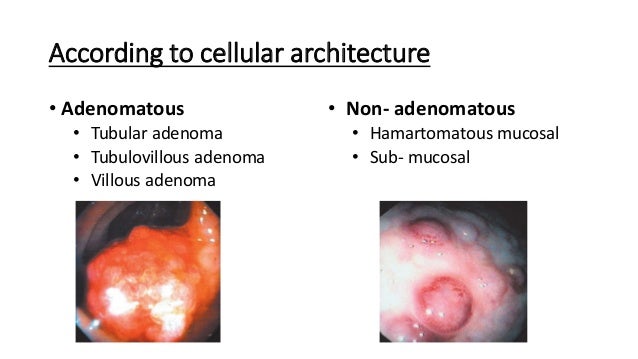
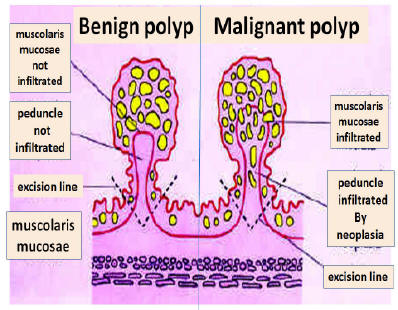
TUBULAR ADENOMAS
most common.
Stalk Fibromuscular tissue Prominent blood vessels from submucosa Usually covered with normal colonic epithelium Polyp neoplastic (dysplastic) epithelium
SESSILE SERRATED polyps
Cancer rare in tubular adenomas < 1 cm Risk in sessile villous adenomas >4 cm up to 40%
ADENOMATOUS polyps

All have epithelial proliferative dysplasia* Ranges from low- to high-grade (carcinoma-in-situ) Strong evidence they are precursor lesions for colorectal adenocarcinoma Estimated that it takes 10 years to double in size
ADENOMATOUS polyps
MC of neoplastic polyps Precursors to adenocarcinoma M>F slightly Common in adults > 60 in developed world.
Most asymptomatic; some bleed ? Adult surveillance beginning age 50? “Patients at increased risk, including those with a family history of colorectal adenocarcinoma, are typically screened by colonoscopy at least 10 years before the youngest age at which a relative was diagnosed”.
Well-defined familial predisposition for development of sporadic adenomas First degree relative 4X increased risk of developing adenomas Also 4X increased risk of developing adenocarcinomas
Peutz-Jeghers syndrome
Arborizing network of connective tissue and smooth muscle which extends into polyp and surrounds epithelium Epithelium composed of normal and abundant intestinal type glands rich in goblet cells
large , pedunculated with firm, lobulated contour
JUVENILE POLYPOSIS syndrome

Most of lesion is stroma(aka lamina propria) Cystically dilated glands Inflammation common Surface eroded or congested with granulation tissue
JUVENILE polyps
juvenile polyps not associated with JPS carry no risk for cancer, but those that do occur with JPS are at increased risk for adenocarcinoma
HAMARTOMATOUS polyps
Most d/t germline mutations in tumor suppressor genes or protooncogenes, thus may have increased risk for carcinoma. Have both stromal & epithelial overgrowth Not neoplasms
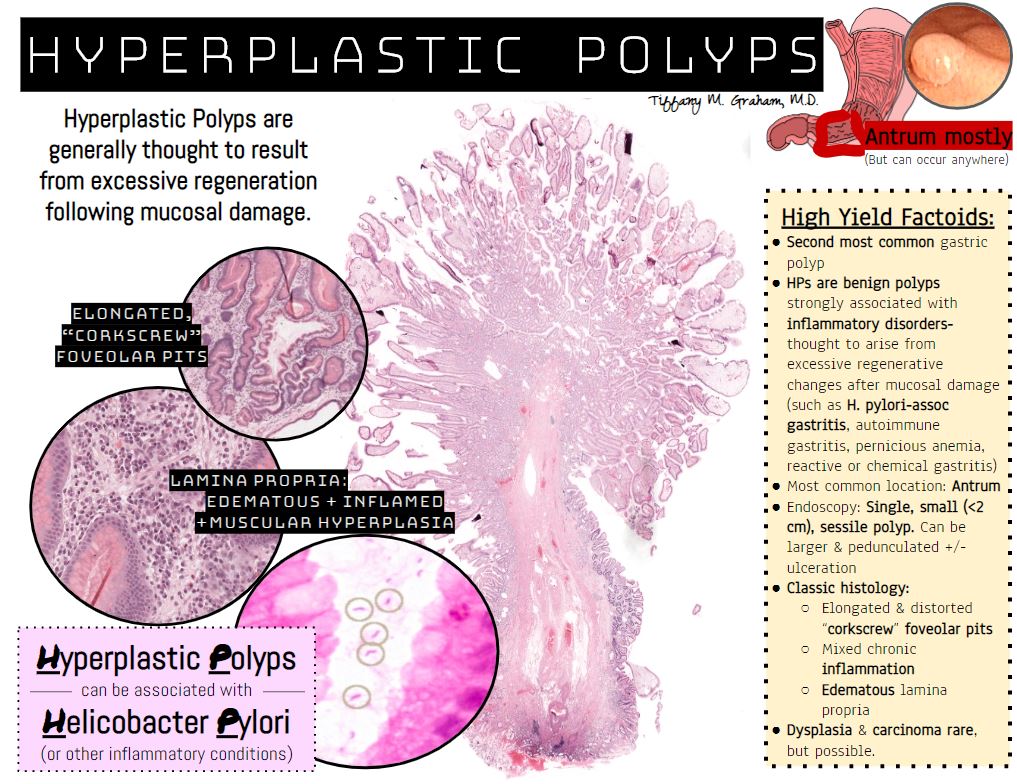
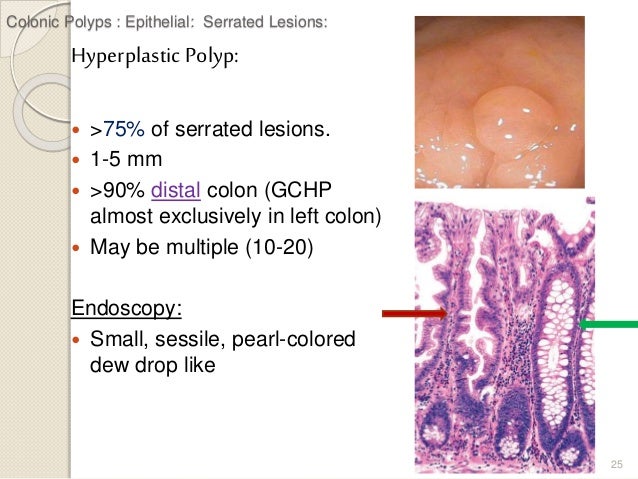
HYPERPLASTIC polyp
Well formed glands and crypts
Lined by non-neoplastic epithelial cells
mature goblet or absorptive cells
Serrated surface glands with irregular crypt architecture
polyps
Tumorous mass that protrudes into lumen
Non-neoplastic: develop secondary to abnormal mucosal maturation(hamartomatous), inflammation(inflammatory polyp), or architecture (hyperplastic polyps)
Majority occur sporadically: Increasing frequency with age Represent 90% of epithelial polyps in colon Majority are hyperplastic Found in more than half of persons over 60 y.o. Inflammatory (pseudo-) polyps: d/t long-standing inflammatory bowel disease (ulcerative colitis, Crohn disease, solitary rectal ulcer syndrome) islands of inflamed, regenerating mucosa surrounded by ulceration and granulation tissue Lymphoid polyps: Essentially normal variants of intramucosal lymphoid tissue resulting in polypoid masses
Neoplastic: epithelium with dysplasia termed adenomatous polyps or adenomas Precursor to cancer MC in colorectal region but may occur in esophagus, stomach or small intestine
carcinoid tumor
Most important prognostic factor in GI carcinoids LOCATION! Location! Location! Foregut carcinoids Stomach, duodenum proximal to ligament of Treitz & esophagus Rarely mets, cured mostly by resection Midgut carcinoids Jejunum & ileum Often multiple, aggressive Greater depth of local invasion, larger size, necrosis & mitoses= worse outcome Hindgut carcinoids Appendix( usually at tip, <2 cm and mostly act B9) & colorectal ( produce polypeptide hormones, serotonin) Usually incidental & small when found
ANGIODYSPLASIA of the GI tract

bowel wall EDEMA
HAMARTOMATOUS polyps

electron microscopy, carcinoid tumor cells

GISTs

on histology, diffuse-type gastric adenocarcinoma cells display “signet rings”
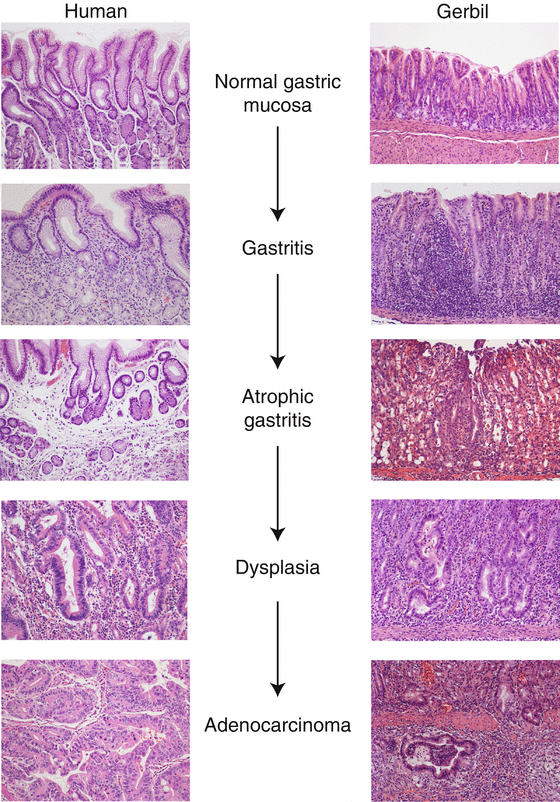
chronic atrophic metaplastic gastritis
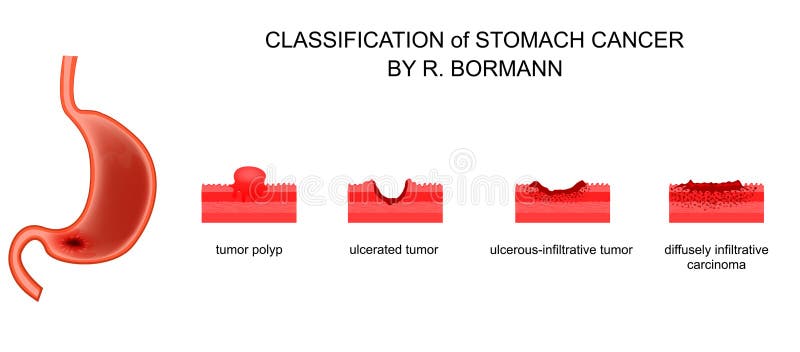
infiltrative growth pattern
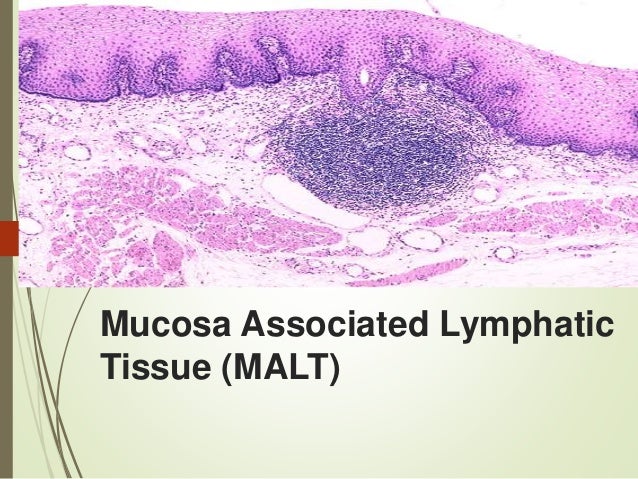
MALT
eosinophilic esophagitis involves epithelial infiltration of eosinophils throughout the esophagus
GERD causes elongation of the papillae

GERD causes elongation of the papillae of the lamina propria and hypertrophy of the basal cells of the mucosa
colon cancer can present with an “apple core” lesion on imaging

Family adenomatous polyposis

sessile, larger than tubular adenomas, long glands with villi-like projections

VILLOUS ADENOMAS

TUBULAR ADENOMAS display round tubular gland cross sections on histology

ADENOMAS with a greater degree of dysplasia

TUBULAR ADENOMAS
ADENOMATOUS polyps
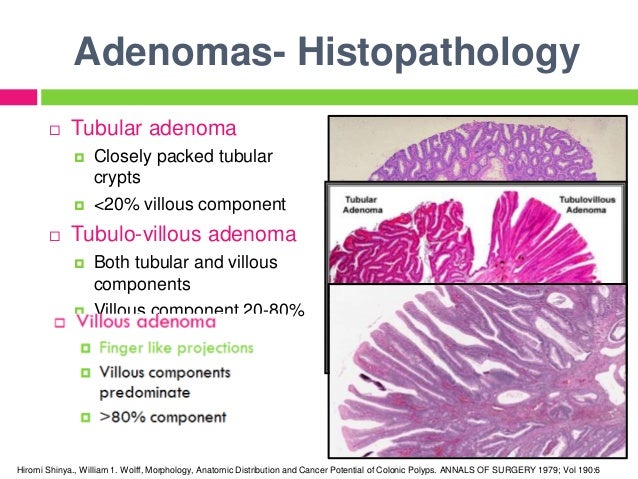
ADENOMAS
SESSILE SERRATED polyp
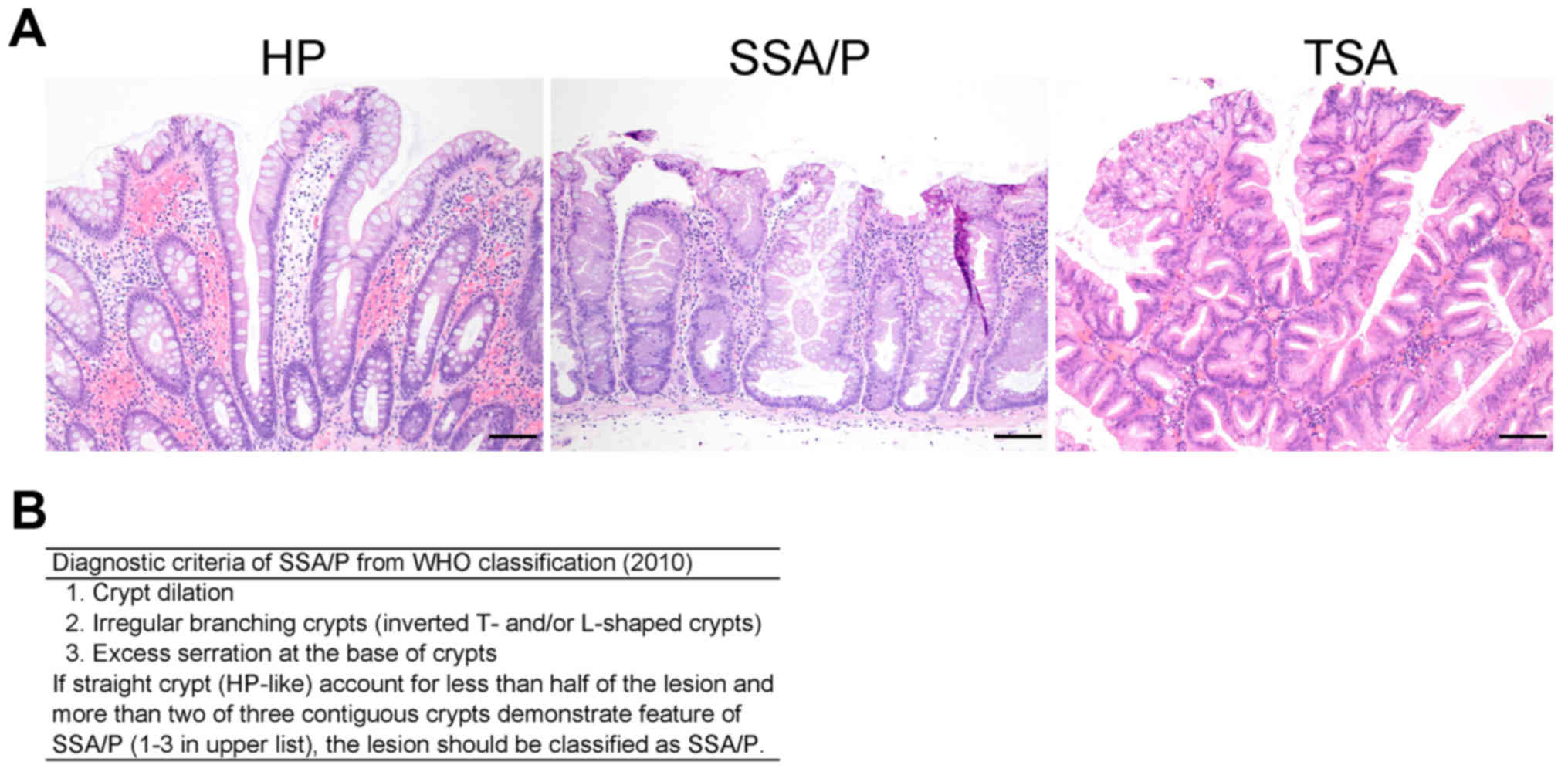 HP, hyperplastic polyp; SSA/P, sessile serrated adenoma/polyp; TSA, traditional serrated polyp
HP, hyperplastic polyp; SSA/P, sessile serrated adenoma/polyp; TSA, traditional serrated polyp
serrated architecture
 Hyperplastic polyp with elongated crypts, serrated architecture in the upper half of the crypts, small, basally placed nuclei without atypia in cytology and architecture
Hyperplastic polyp with elongated crypts, serrated architecture in the upper half of the crypts, small, basally placed nuclei without atypia in cytology and architecture
abundant goblet cells
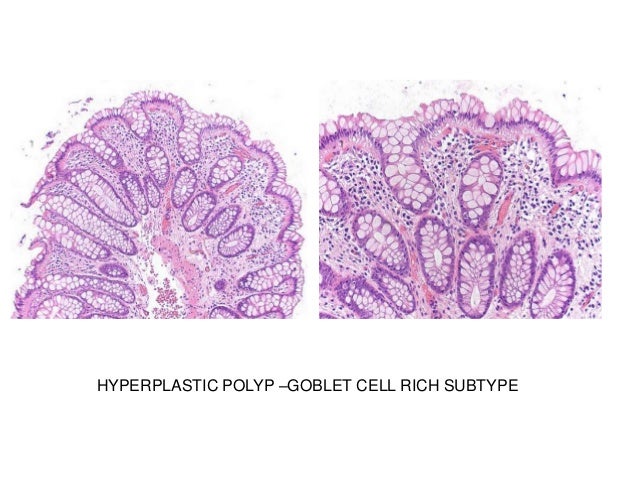
HYPERPLASTIC polyp
small cystic spaces (glands filled with mucin and debris)

JUVENILE polyps
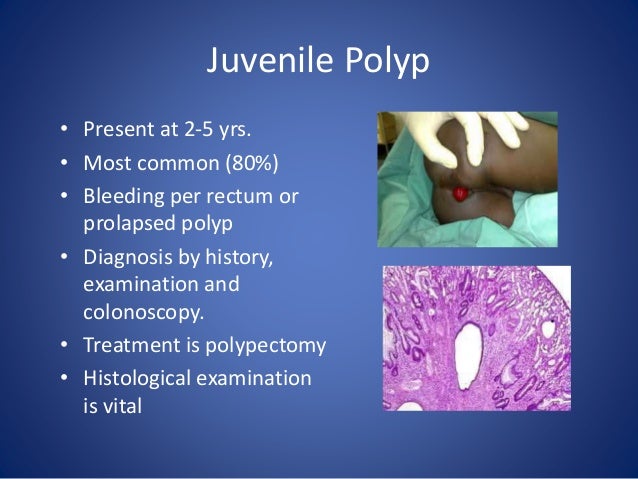
JUVENILE POLYPOSIS syndrome

may be neoplastic or non-neoplastic
neoplastic or non-neoplastic

polyps

colon

pedunculated or sessile

polyps
HAMARTOMATOUS polyps

symptoms include fever, rigidity, mental status changes, autonomic instability, rhabdomyolysis

neuroleptic malignant syndrome
mesenteric roots
The root of the mesentery, or root of the small bowel mesentery to be exact, is the origin of the mesentery of the small intestine (i.e. jejunum and ileum) from the posterior parietal peritoneum., attached to the posterior abdominal wall. It extends from the duodenojejunal flexure to the ileocecal junction in the right iliac fossa.
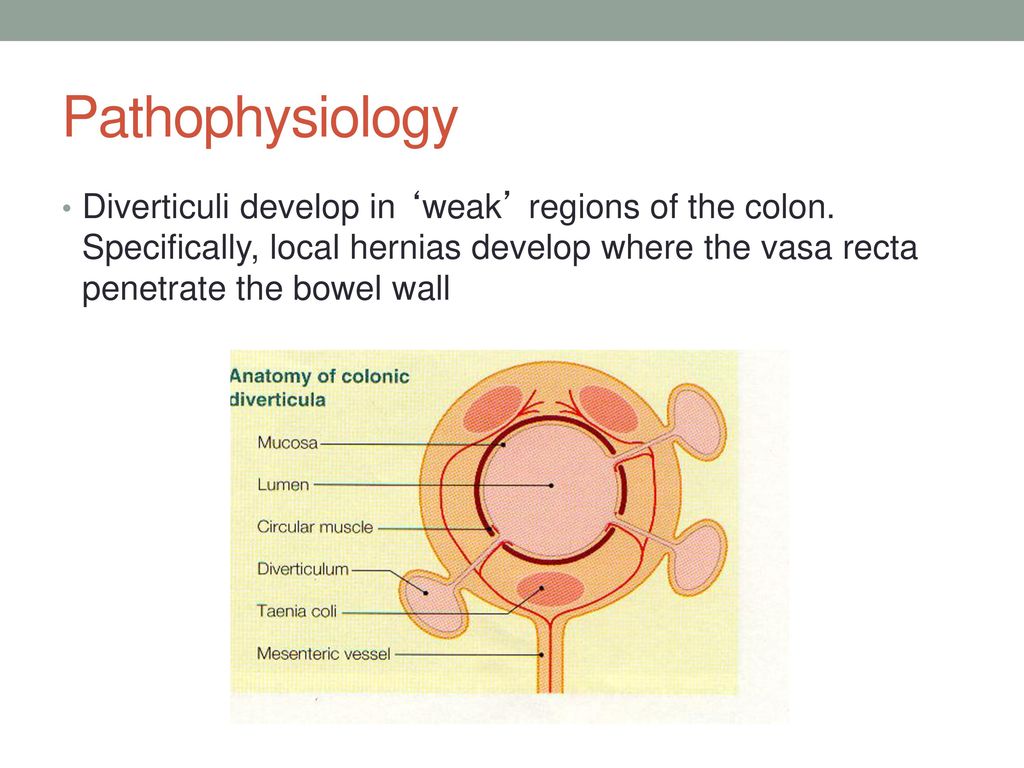
vasa recta arteries penetrate the muscularis at the mesenteric border
Annular fissures (tears)
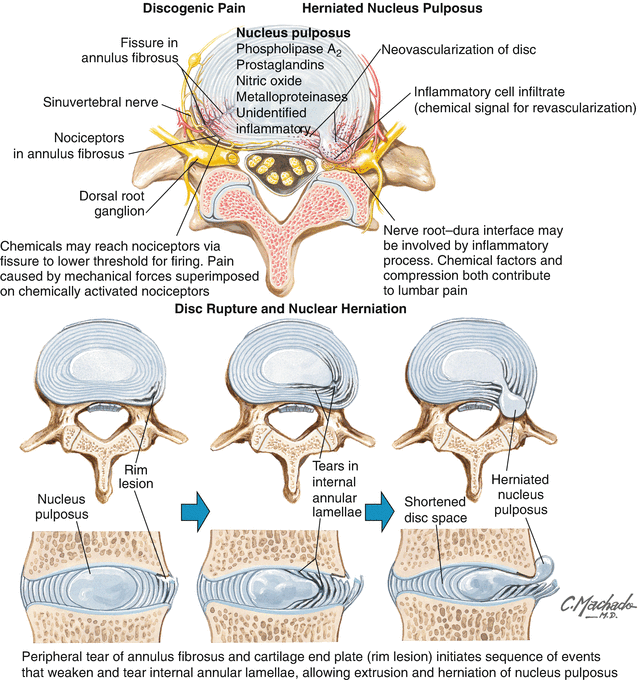
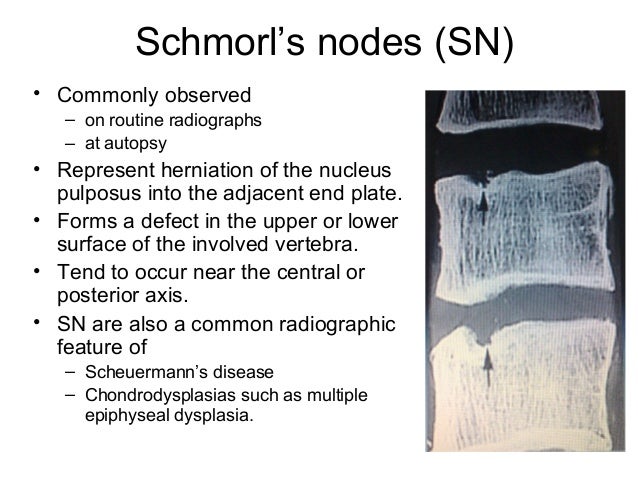
Schmorl's nodes
spondylosis
Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related wear and tear of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints (facet syndrome). If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.
radicular pain
When the radiating pain is associated with numbness or weakness, the diagnosis is radiculopathy if the lesion is at the nerve root and myelopathy if at the spinal cord itself.
Epidural abscess
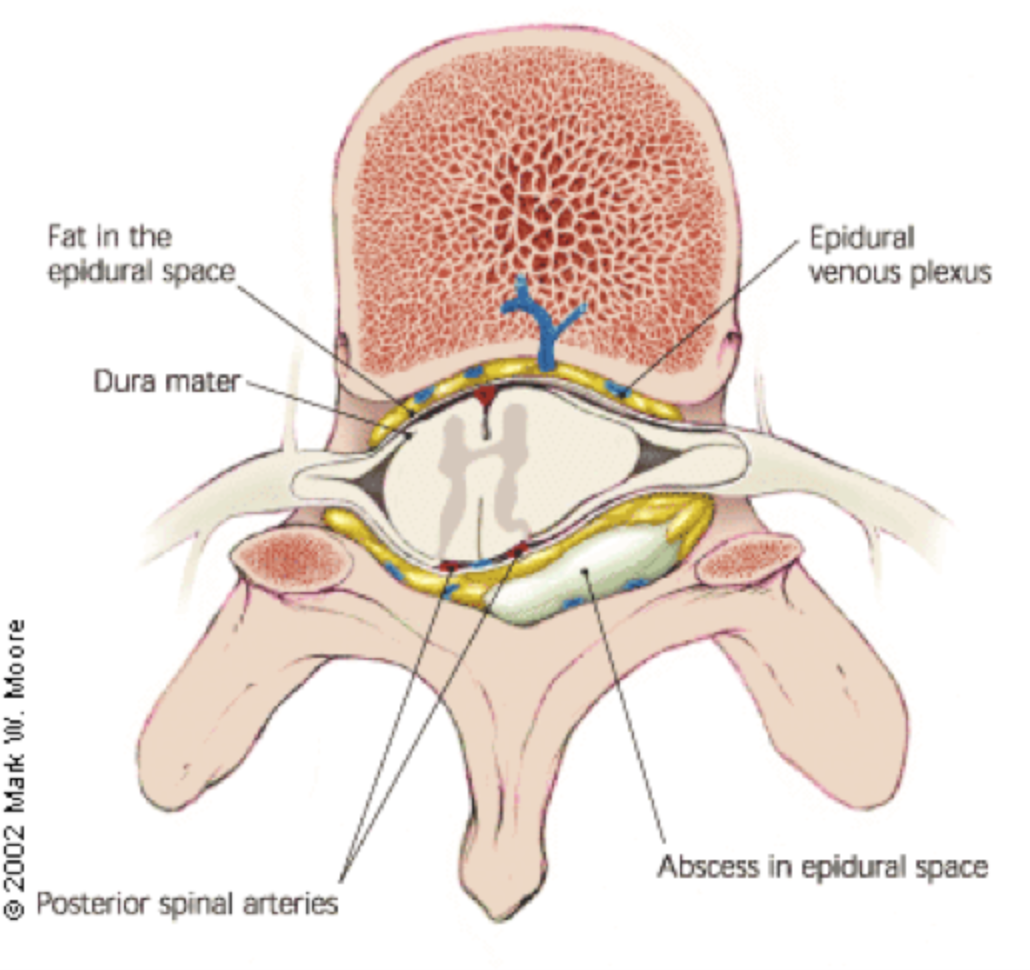
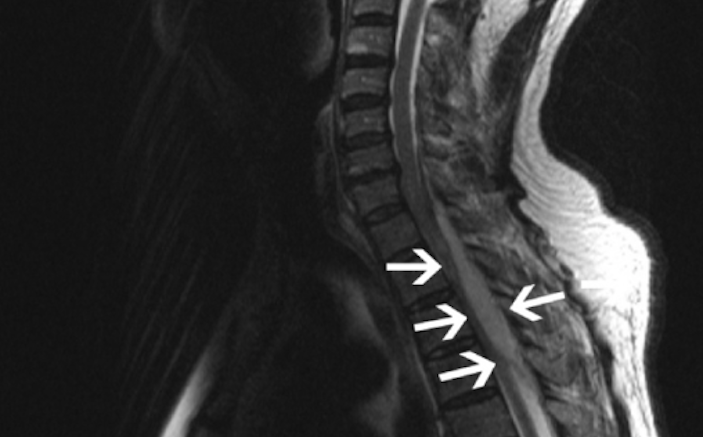 Spinal epidural abscesses usually occur in the thoracic or lumbar regions. An underlying infection is often present; it may be remote (eg, endocarditis, furuncle, dental abscess) or contiguous (eg, vertebral osteomyelitis, pressure ulcer, retroperitoneal abscess). In about one third of cases, the cause cannot be determined. The most common causative organism is Staphylococcus aureus, followed by Escherichia coli and mixed anaerobes.
Spinal epidural abscesses usually occur in the thoracic or lumbar regions. An underlying infection is often present; it may be remote (eg, endocarditis, furuncle, dental abscess) or contiguous (eg, vertebral osteomyelitis, pressure ulcer, retroperitoneal abscess). In about one third of cases, the cause cannot be determined. The most common causative organism is Staphylococcus aureus, followed by Escherichia coli and mixed anaerobes.
facet hypertrophy
The facet joint may become enlarged as part of the body's response to degeneration of the spine, i.e. to try to provide additional stability to counteract the instability from degenerative disc disease.
The joint can enlarge to the point where it puts pressure on the adjacent nerves in the spine, which in turn can cause pain to radiate along the path of the nerve Lumbar spinal canal stenosis (LSCS) results from degenerative changes in the spinal canal and is one of the most common spinal disorders in elderly individuals. characterized by narrowing of the spinal canal caused by hypertrophy of the ligamentum flavum, mechanical compression of the lumbar spinal nerve roots, and disc herniation combined with osteophytes Facet joint hypertrophy (FJH) is considered another major cause of LSCS