Dr Ellie Murray [@EpiEllie] (2020-08/18) Sneak peek: I’m doing a Reddit #AMA on Aug 27! I’m a total Reddit newbie. What do I need to know? Twitter
- Jan 2021
-
twitter.com twitter.com
-
news.sky.com news.sky.com
-
Science says the risk of transmission outdoors is roughly 20 times lower than it is inside.Even a faint breeze helps to disperse most virus particles that hang in the air.The risk is low, but it's not zero.
-
-
psyarxiv.com psyarxiv.com
-
Masuyama, A., Kubo, T., Sugawara, D., & Chishima, Y. (2020). Interest consistency can buffer the effect of COVID-19 fear on psychological distress. PsyArXiv. https://doi.org/10.31234/osf.io/ygz37
-
-
-
Smith, R., Myrick, J. G., Lennon, R. P., Martin, M. A., Small, M. L., Scoy, L. J. V., & Group, D. R. (2020). Optimizing COVID-19 Health Campaigns: A Person-Centered Approach. PsyArXiv. https://doi.org/10.31234/osf.io/xuefh
-
-
apps.who.int apps.who.int
-
Organization, W. H. (2020). Behavioural considerations for acceptance and uptake of COVID-19 vaccines: WHO technical advisory group on behavioural insights and sciences for health, meeting report, 15 October 2020. World Health Organization. https://apps.who.int/iris/handle/10665/337335
-
-
reutersinstitute.politics.ox.ac.uk reutersinstitute.politics.ox.ac.uk
-
As vaccines start rolling out, here’s what our research says about communication and coronavirus. (n.d.). Reuters Institute for the Study of Journalism. Retrieved 13 January 2021, from https://reutersinstitute.politics.ox.ac.uk/risj-review/vaccines-start-rolling-out-heres-what-our-research-says-about-communication-and
-
-
-
Despite some implementation challenges, patient portals have allowed millions of patients to access to their medical records, read physicians’ notes, message providers, and contribute valuable information and corrections.
I wonder if patients have edit - or at least, flag - information in their record?
-
- Dec 2020
-
twitter.com twitter.com
-
Bu Experts {@BU Experts} (2020) How can we navigate daily life during the pandemic? #Publichealth expert & epidemiologist @EpiEllie will be on @reddit_AMA this Thursday (8/27) at 12pm ET to answer all of your #COVID19-related questions. She'll discuss how to safely see friends and family, travel & more. @BUSPH. Twitter. Retrieved from: https://twitter.com/BUexperts/status/1297932614909792258
-
-
zeynep.substack.com zeynep.substack.com
-
People who think that racial differences are all biological might say that all these non-White groups have suffered so much excess death because of that bottom circle, because of greater biological susceptibility. Recent studies have evaluated this hypothesis and found that it’s not true. Instead the answer is simpler: Black and Latino/a people in particular are dying of COVID-19 at such staggering rates because they are more likely to be exposed to the virus in infectious settings, particularly workplaces.
-
-
twitter.com twitter.com
-
WearingisCaring {@WearingisCaring} (2020) How can you safely take off your mask? Simply follow these four easy steps to prevent catching the virus! Twitter. Retrieved from: https://twitter.com/WearingisCaring/status/1295707116880134145
-
-
psyarxiv.com psyarxiv.com
-
Weiskittle, R. E., Mlinac, M., & Nicole Downing, L. (2020, August 25). Addressing COVID-19 Worry and Social Isolation in Home-Based Primary Care. https://doi.org/10.31234/osf.io/483zv
-
-
www.nature.com www.nature.com
-
Allen. W. E. (2020) Population-scale longitudinal mapping of COVID-19 symptoms, behaviour and testing. Nature human behaviour. Retrieved from: https://www.nature.com/articles/s41562-020-00944-2?utm_source=feedburner&utm_medium=feed&utm_campaign=Feed%3A+nathumbehav%2Frss%2Fcurrent+%28Nature+Human+Behaviour%29
-
-
-
When they did pay attention, they invariably blamed the victims — their “unhealthy” behaviors and diets, their genes, the under-resourced neighborhoods they “chose” to live in and the low-paying jobs they “chose” to work. Their chronic illnesses were seen as failures of personal responsibility. Their shorter life expectancy was written off to addiction and the myth of “black-on-black” violence. Many of those arguments were legacies of the slave and Jim Crow eras, when the white medical and science establishment promoted the idea of innate Black inferiority and criminality to rationalize systems built on servitude and segregation.
Is this an example of de jure or de facto racism and discrimination? Explain your thinking.
-
public health experts mostly ignored the disparities
Who do you think these experts were? How might that have changed?
Tags
Annotators
URL
-
-
wwwnc.cdc.gov wwwnc.cdc.gov
-
Evidence and experience suggest that in pandemic phase 6 (increased and sustained transmission in the general population), aggressive interventions to isolate patients and quarantine contacts, even if they are the first patients detected in a community, would probably be ineffective, not a good use of limited health resources, and socially disruptive.
Ontario going in lockdown after the 26 December.
-
Field studies coordinated by WHO will be needed to assess virus transmission characteristics, amplifying groups (e.g., children vs. adults), and attack and death rates. Information on these factors will be needed urgently at the onset of a pandemic because the pandemic subtype may behave differently than previous pandemic or seasonal strains. Such studies will also be needed throughout the pandemic period to determine if these factors are changing and, if so, to make informed decisions regarding public health response measures, especially those that are more costly or disruptive.
Public Health Ontario are you following this? If this is not the case the entire "brain trust" should summarily dismissed.
-
-
www.nature.com www.nature.com
-
Ledford, H., Cyranoski, D., & Noorden, R. V. (2020). The UK has approved a COVID vaccine—Here’s what scientists now want to know. Nature, 588(7837), 205–206. https://doi.org/10.1038/d41586-020-03441-8
-
-
-
blue light has been found to have the strongest impact on your natural production of melatonin, filtering it out when you’re using devices at night can make it easier to fall asleep, according to a recent study published in the Journal of Applied Psychology. But even here, experts see a more mundane connection between devices and comfort: “Most of the negative impact of electronics on sleep and on your circadian clock is not due to the light. It’s due to the fact that these things are engineered to keep you awake and entertained and engaged in what you’re doing for an extended period of time,”
Finding it hard to sleep might be either because of the blue light or the psychological effect of screens on us
-
Reynolds encourages following the 20-20-20 rule: “Take a 20-second break to view something 20 feet away every 20 minutes.”
20-20-20 rule (screen-free break technique)
-
The American Academy of Ophthalmology asserts that dry eyes are more likely to be the result of decreased blinking. The AAO asserts that people blink 15 times per minute in normal circumstances (“normal” being relative, here) but only five to seven times per minute while staring at a screen. Solutions for preventing dry eyes can be as simple as reminding yourself to blink, or using artificial tear drops throughout your day as a preventive measure. It’s also possible that you’re blinking even less if your superclose to your screen.
The true reason of dry eyes: rare blinking
-
-
-
How We Can Stop the Spread of Coronavirus by Christmas. (n.d.). Time. Retrieved December 17, 2020, from https://time.com/5912705/covid-19-stop-spread-christmas/
-
-
www.nature.com www.nature.com
-
Marshall. M., (2020) How COVID-19 can damage the brain. nature. Retrieved from:https://www.nature.com/articles/d41586-020-02599-5?utm_source=twt_nnc&utm_medium=social&utm_campaign=naturenews&sf237834255=1
-
-
twitter.com twitter.com
-
ReconfigBehSci {@SciBeh} (2020) The pandemic proves we all should know ‘psychological first aid.’ Here are the basics. /lifestyle/wellness/pandemic-psychological-first-aid-anxiety/2020/09/21/7c68d746-fc23-11ea-9ceb-061d646d9c67_story.html?tid=ss_tw. Twitter. Retrieved from: https://twitter.com/SciBeh/status/1308461925785837573
-
-
www.latimes.com www.latimes.com
-
The official definition of a “close contact” — 15 minutes, within six feet — isn’t foolproof.
The takeaway: The official definition of a "close contact" for COVID-19 is not foolproof.
The claim: The official definition of a "close contact" - 15 minutes, within six feet - isn't foolproof.
The evidence: In Korea, a person sitting in a restaurant 6.5 meters (>20ft) away from the COVID index case for five minutes was infected, most likely because airflow from the air conditioner carried droplets with COVID-19 from the infected person to the person who became infected (1). How common transmission across large distances occurs is still debated (2). As several indoor outbreaks were attributed to airborne transmission, precautions to prevent airborne COVID transmission are needed (3). Examples include better air filtration/UV to kill virus in the system, increased air flow from outside, avoidance of recirculating interior air, and avoiding overcrowding in interior spaces.
Sources:
1) https://jkms.org/DOIx.php?id=10.3346/jkms.2020.35.e415
2) https://www.sciencedirect.com/science/article/pii/S0166093420302858?via%3Dihub
3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7454469/pdf/ciaa939.pdf
-
-
www.scientificamerican.com www.scientificamerican.com
-
Achakulwisut, P. (n.d.). The U.S. Risks Locking In a Climate Health Crisis in Response to COVID. Scientific American. Retrieved December 10, 2020, from https://www.scientificamerican.com/article/the-u-s-risks-locking-in-a-climate-health-crisis-in-response-to-covid/
-
-
www.facebook.com www.facebook.com
-
(4) Facebook. (n.d.). Retrieved December 10, 2020, from https://www.facebook.com/harvardpublichealth/videos/881117569360098/
-
-
psyarxiv.com psyarxiv.com
-
Sisson, N. M., Willroth, E. C., Le, B. M., & Ford, B. Q. (2020, December 1). The Mental Health Effects of Living with Close Others Before, During, and After the Onset of COVID-19. https://doi.org/10.31234/osf.io/v9mc4
-
-
-
Cameron, E. E., Joyce, K. M., Rollins, K., & Roos, L. E. (2020, November 29). Paternal Depression & Anxiety During the COVID-19 Pandemic. https://doi.org/10.31234/osf.io/drs9u
-
-
gbdeclaration.org gbdeclaration.org
-
Adopting measures to protect the vulnerable should be the central aim of public health responses to COVID-19.
Public health departments world wide are failing.
-
Current lockdown policies are producing devastating effects on short and long-term public health. The results (to name a few) include lower childhood vaccination rates, worsening cardiovascular disease outcomes, fewer cancer screenings and deteriorating mental health – leading to greater excess mortality in years to come, with the working class and younger members of society carrying the heaviest burden.
The cure is worse than the disease.
Tags
Annotators
URL
-
-
psyarxiv.com psyarxiv.com
-
Długosz, P. (2020). Factors influencing mental health among American youth in the time of the Covid-19 pandemic. PsyArXiv. https://doi.org/10.31234/osf.io/8npyc
-
- Nov 2020
-
psyarxiv.com psyarxiv.com
-
Marmet, S., Wicki, M., Gmel, G., Gachoud, C., Daeppen, J.-B., Bertholet, N., & Studer, J. (2020). The psychological impact of the COVID-19 crisis on young Swiss men participating in a cohort study. PsyArXiv. https://doi.org/10.31234/osf.io/kwxhd
-
-
www.acpjournals.org www.acpjournals.org
-
The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use.
The takeaway: While minimal protection occurs when a mask is worn in a place where many others are not wearing a mask, community masking is associated with a reduction in COVID cases.
The claim: In a community with modest infection rates, some social distancing, and most people not wearing masks, wearing a surgical mask did not reduce the SARS-CoV-2 infection rate by more than 50%.
The evidence: This study showed that wearing a mask in a community where most people did not wear a mask, did not reduce the risk of getting infected by 50%. Fewer COVID infections were reported in the mask group than in the unmasked group. This study agrees with a meta analysis which showed that masks resulted in a decrease in infections but did not prevent all infections (1) According to the CDC, seven studies have shown community level benefit when masking recommendations were made (2).
When most in the community are not wearing masks, social distancing, and washing hands, wearing a mask alone provides minimal protection to the mask wearer. Community wide masking is associated with a reduction in COVID cases (2).
Sources:
1) https://pubmed.ncbi.nlm.nih.gov/29140516/
2) https://www.cdc.gov/coronavirus/2019-ncov/more/masking-science-sars-cov2.html
-
-
-
Study of patients attending a hospital-based obesity service shows no difference in weight loss between those under 60 years old and those from 60 to 78 years old The University of Warwick-led study conducted at University Hospitals Coventry and Warwickshire (UHCW) concludes that lifestyle changes to manage weight loss are effective in reducing obesity regardless of age Aims to dispel myths about effectiveness of weight loss in older people
- Researchers studied 242 patients (under 60 and over 60 years old) who attended a weight-loss programme, most of them morbidly obese.
- Results show no differences between age groups, proving that weight loss is as important for older people - even more so - as for younger people.
- The programme was based on lifestyle-based changes - diet, physical activity and psychological support - and showed similar results regardless of age.
- People often don’t care about weight loss in older people, and this study shows that it’s a very harmful perspective to adopt.
-
-
www.independent.co.uk www.independent.co.uk
-
Human ageing reversed in ‘Holy Grail’ study, scientists say
- Clinical trial with 35 people over 64 years old shows that oxygen therapy can reverse two key indicators of biological ageing - telomere length, and senescent cells.
- Telomeres are protective caps at the end of chromosomes, and senescent cells are malfunctioning, old cells.
- Patients were placed in a pressurised chamber and given pure oxygen for 90 minutes a day, 5 days a week, for 3 months.
- At the end, telomere length increased by 20% on average, and senescent cells were reduced by 37% - equivalent to a 25 years younger biological-cellular state.
- The results are incomparable to lifestyle changes / exercise / diets, and researchers say it’s thanks to inducing cell regeneration through hypoxia (oxygen shortage).
-
-
www.blinkist.com www.blinkist.com
-
You can find your mental health triggers by beginning a thought diary
A Thought Diary will help you find triggers when you write down things that went wrong and your accompanying feelings.
An example would be how not meeting a deadline made you feel. What happened right after you realized you didn't meet the deadline?
-
The best course of action is to discreetly arrange a one-to-one meeting, and sensitively explore how he’s feeling. It can be useful to write a wellness action plan together. This is a document in which the employee writes down information about the mental-health problems he’s experiencing, and what triggers exist in his workplace that contribute to these feelings. You can then draw up a strategy together for how to help him improve his mental health in the workplace, and make a list of actions that both of you can take to help get him back on track.
A manager can sit down with the affected employee and write an wellness action plan. This will include:
- Employee's mental health problems
- Triggers within the workplace
- A strategy to work together with employee to help them improve in the workplace.
- A list of actions that can be done. e.g. Counseling, reduce working time, set limits with coworkers
-
-
psyarxiv.com psyarxiv.com
-
Mulukom, V. van, Pummerer, L., Alper, S., Bai, (Max) Hui, Cavojova, V., Farias, J. E. M., Kay, C. S., Lazarevic, L., Lobato, E. J. C., Marinthe, G., Banai, I. P., Šrol, J., & Zezelj, I. (2020). Antecedents and consequences of COVID-19 conspiracy theories: A rapid review of the evidence. PsyArXiv. https://doi.org/10.31234/osf.io/u8yah
-
-
www.sciencemag.org www.sciencemag.org
-
CohenNov. 16, J., 2020, & Am, 7:00. (2020, November 16). ‘Just beautiful’: Another COVID-19 vaccine, from newcomer Moderna, succeeds in large-scale trial. Science | AAAS. https://www.sciencemag.org/news/2020/11/just-beautiful-another-covid-19-vaccine-newcomer-moderna-succeeds-large-scale-trial
Tags
- Pfizer
- lang:en
- COVID-19
- BioNTech
- is:webpage
- distribution
- optimism
- trial
- health
- efficacy
- Moderna
- mRNA technology
- vaccine
- USA
Annotators
URL
-
-
psyarxiv.com psyarxiv.com
-
Agarwal, A. (2020). Ripple Effect of a Pandemic: Analysis of the Psychological Stress Landscape during COVID19. PsyArXiv. https://doi.org/10.31234/osf.io/nat49
-
-
www.samaritans.org www.samaritans.org
-
Samaritans responds to NCISH’s 2020 suicide figures in England. (n.d.). Samaritans. Retrieved 18 November 2020, from https://www.samaritans.org/news/samaritans-responds-ncish-new-suicide-figures-england/
-
-
www.justfacts.com www.justfacts.com
-
Anxiety From Reactions to Covid-19 Will Destroy At Least Seven Times More Years of Life Than Can Be Saved by Lockdowns
Take away: Though the number of COVID deaths prevented and the exact number of years lost due directly to decreases in mental health from lockdowns is at best a rough estimate, several facts are known. Lockdowns decrease mental health, and a decrease in mental health shortens lives too.
The claim: Anxiety from reactions to COVID-19 will destroy at least seven times more years of life than can be saved by lockdowns.
The evidence: This article references many studies detailing the anxiety surrounding COVID-19 (1-4). These studies indicate that many people have increased stress due to COVID. Nature Public Health Emergency Collection reports that the mental health cost of widespread lockdowns may negate the lives saved by this policy (5). This article lists many articles which describe the effect of stay-at-home orders on mental health. Additionally, the effect of poor mental health on physical outcomes is well-defined. Poor mental health shortens lives. Other factors with COVID such as negative media coverage and dealing with job loss and death are also described as negatively affecting mental health. It is unclear how much of the negative mental health outcomes is directly related to lockdowns and what is contributed to the disease, job loss, future uncertainty, and continuous media coverage.
Several supporting facts used in this article are now outdated or could use clarification. Many assumptions are detailed in this article to estimate the number of years lost due to mental harm caused by lockdowns. One example is the authors used a survey of 1,266 patients to estimate the number of people in the United States who have suffered mental harm from lockdowns. These estimates are challenging to conclusively verify. The authors did choose the conservative estimate for each of their numbers. One example of an outdated number is the predicted number of deaths was 114,228 by August 4th. The actual number of deaths per Johns Hopkins was 157,500 (6).
Based on the facts, anxiety and mental disorders can be deadly. Lockdowns result in an increase in poor mental health. The exact number of years lost due to poor mental health directly resulting from lockdowns is less clear. Poor mental health may also result from constant media coverage, loss of loved ones and fear of the future.
The sources:
2) https://www.kff.org/health-reform/report/kff-health-tracking-poll-early-april-2020/
-
-
codescene.com codescene.com
-
Refactoring at scale is challenging and a significant investment, so communicating the progress is important both from a business perspective but also as a motivational effect to developers. In this case we used a combination of complexity trend visualizations and Code Health Metric as shown in the preceding example.
[[refactoring at scale]]
-
-
www.weforum.org www.weforum.org
-
3. They're fighting misinformation.
Agree or disagree with how they obtained info and what that means for digital rights; how much the Chinese government informed or not their people - this is what China did in terms of alerting their population of covid cases.
-
-
www.theguardian.com www.theguardian.com
-
mink are now considered a public health risk
Takeaway: Mink are capable of contracting and transmitting SARS-CoV-2 to each other and to humans which had resulted in mutated SARS-CoV-2.
The claim: Mink are now considered a public health risk.
The evidence: SARS-CoV-2 infects and kills mink (1). The lung damage in mink from SARS-CoV-2 is similar to the damage in human lungs from SARS-CoV-2. The range of symptoms from asymptomatic to deadly is exhibited by the mink. Based on this pre-print article, SARS-CoV-2 is mutating in mink farms and had documented transmission from mink to humans (2).
Extensive sequencing of SARS-CoV-2 genomes has been done (3). Mutations tend to occur in certain hot spots of the genome. The stated purpose of the sequencing research is to identify relatively stable parts of the genome to use as vaccine targets to help avoid mutant escape. The genomes of SARS-CoV-2 from mink infections had more nucleotide differences than SARS-CoV-2 from human COVID outbreaks (2). This may be due to a faster mutation rate or to the fact that so many mink were infected.
Sources:
2) https://www.biorxiv.org/content/10.1101/2020.09.01.277152v1
-
-
-
What are the main trends in medical mobile app development and how to to build a healthcare app to get the best results. We highlight the general insights of the business and technical models of mobile healthcare apps.
-
- Oct 2020
-
www.livescience.com www.livescience.com
-
We found that those medications, some of them at least 40 years past their manufacture date, still retained full potency
-
-
-
Experts say closing borders early and tightly regulating travel have gone a long way toward fighting the virus. Other factors include rigorous contact tracing, technology-enforced quarantine and universal mask wearing. Further, Taiwan’s deadly experience with SARS has scared people into compliance.
The Takeaway: The combination of closing borders, tightly regulating travel, effective quarantine of all exposed people using cell phone data for enforcement, and universal mask wearing contributed to effectively keeping COVID-19 from infecting most of Taiwan's population.
The claim: Closing borders early, tightly regulating travel, contact tracing, technology-enforced quarantine, universal mask wearing, and Taiwan's previous deadly experience with SARS resulted in control of SARS-CoV-2 in Taiwan.
The evidence: The earlier COVID-19 cases are stopped from entering a country, the fewer cases will be present to spread the disease to others. To illustrate, it is easier to stop a trickle of water than to try to dam up a flood and easier to extinguish a candle than a forest fire. Taiwan closed its borders on January 23rd, 2020 (1). The Philippines closed their borders on February 2nd, 2020 (2). Tightly regulating travel will help to stop cases before they enter the country. Effective quarantining the few cases and contacts of the cases which do enter a country is critical to preventing the spread of the disease within the country. Taiwan used mobile telephone data to enforce quarantine (1). Without quarantine, each infected person will spread COVID-19 to 2-6 additional people based on the R0 (3, 4). Universal masking will help slow the spread of disease (5). Previous experience with controlling a deadly disease will most likely increase compliance to methods to control the disease.
Per Our World in Data website, Taiwan had one of the least stringent government responses to COVID-19 (6). The biweekly number of COVID-19 cases in Taiwan was 23 on October 29, 2020 (7). Neighboring countries had biweekly COVID-19 cases of 372 (China), 28,644 (Philippines), 11,871 (Malaysia), 51 (Vietnam), and 8,142 (Japan). These neighboring countries had more stringent government responses to COVID-19 (6).
Sources:
1) https://focustaiwan.tw/society/202001230011
3) https://pubmed.ncbi.nlm.nih.gov/32234343/
4) https://pubmed.ncbi.nlm.nih.gov/32097725/
5) https://www.nature.com/articles/s41591-020-1132-9#annotations:7jRWRheWEeuY8x_rXDuRjg
6) https://ourworldindata.org/grapher/covid-stringency-index
7) https://ourworldindata.org/grapher/biweekly-confirmed-covid-19-cases
-
-
www.youtube.com www.youtube.com
-
The impact of Covid-19 on media – rise of infodemics? (2020, September 16). https://www.youtube.com/watch?v=QapwrR9C3Z4&feature=youtu.be&ab_channel=InternationalDayofDemocracyEU
-
-
www.youtube.com www.youtube.com
-
COVID-19: The 9/11 Moment for Global Public Health? Dr. Richard Horton and Clive Cookson. (2020, September 1). https://www.youtube.com/watch?v=97iJIwBQ5qE&feature=youtu.be
-
-
www.bbc.co.uk www.bbc.co.uk
-
Covid: Scots told to prepare for “digital Christmas.” (2020, October 22). BBC News. https://www.bbc.co.uk/news/uk-scotland-54643340
-
-
twitter.com twitter.com
-
Jeremy Farrar on Twitter. (n.d.). Twitter. Retrieved October 28, 2020, from https://twitter.com/JeremyFarrar/status/1318983210282459136
-
-
www.theguardian.com www.theguardian.com
-
Geddes, L. (2020, October 21). Women aged 50-60 at greatest risk of ‘long Covid’, experts suggest. The Guardian. https://www.theguardian.com/world/2020/oct/21/women-aged-50-60-at-greatest-risk-of-long-covid-experts-suggest
-
-
www.thelocal.se www.thelocal.se
-
What you need to know about Sweden’s new local coronavirus recommendations. (2020, October 19). https://www.thelocal.se/20201019/what-you-need-to-know-about-swedens-new-local-coronavirus-recommendations
-
-
www.channel4.com www.channel4.com
-
‘Bus drivers didn’t have adequate PPE even though they requested it’ – Edinburgh University’s Dr Gwenetta Curry. (2020, October 19). Channel 4 News. https://www.channel4.com/news/bus-drivers-didnt-have-adequate-ppe-even-though-they-requested-it-edinburgh-universitys-dr-gwenetta-curry
Tags
- occupational risk
- transmission
- lang:en
- video
- COVID-19
- protective equipment
- public health
- is:news
- bus driver
- safety
- request
- concern
Annotators
URL
-
-
twitter.com twitter.com
-
Rent Strike Bristol on Twitter. (n.d.). Twitter. Retrieved October 27, 2020, from https://twitter.com/RentStrikeBris/status/1317073795291729921
-
-
-
Dennis, A., Wamil, M., Kapur, S., Alberts, J., Badley, A. D., Decker, G. A., Rizza, S. A., Banerjee, R., Banerjee, A., & Investigators, O. behalf of the C. study. (2020). Multi-organ impairment in low-risk individuals with long COVID. MedRxiv, 2020.10.14.20212555. https://doi.org/10.1101/2020.10.14.20212555
-
-
twitter.com twitter.com
-
Royal Statistical Society on Twitter. (n.d.). Twitter. Retrieved October 25, 2020, from https://twitter.com/RoyalStatSoc/status/1317133702183456769
-
-
journals.sagepub.com journals.sagepub.com
-
Structural Racism as SDH: -Examples: 1) Home Health workers not eligible for paid leave causing disproportionate harm when injured 2) Nursing Home: SSA funded private long term care for the elderly and prohibited funding for institutions for AA individuals Laws 1) Often don't address root causes. For example, anti-discrimination laws legitimizes existing structures
-
-
unglobalcompact.org unglobalcompact.org
-
But that could be a drop in the ocean compared to the humanitarian fallout. “We’ve seen 400,000 die from COVID-19,” David Beasley, the Executive Director of the World Food Programme, warned in June. “We could see 300,000 die a day, for several months, if we don’t handle this right.”
Take away: The humanitarian fallout from prolonged lockdowns to control COVID-19 could be worse than the deaths due to COVID-19.
The claim: The humanitarian fallout from COVID-19 could be worse than the deaths caused directly by the disease.
The evidence: Food supply chains have been disrupted due to COVID-19 (1). The World Health Organization predicts that 130 million additional people could become chronically hungry due to COVID-19 (2). Per the International Labor Organization, 1.6 billion workers have the prospect of their employment destroyed, at least partially due to the prolonged lockdowns (3).
“For millions of workers, no income means no food, no security and no future. [...] As the pandemic and the jobs crisis evolve, the need to protect the most vulnerable becomes even more urgent."
Guy Ryder, ILO Director-General
A number of socio-economic consequences have resulted from COVID-19 lock-down measures to control the virus (4). 900 million learners are affected by lockdowns which results in high risk children lacking access to free meals provided by school systems, drop out rates, and social isolation/mental health (4). Affects have been seen in the agricultural, manufacturing, petroleum and oil, finance industry, travel and aviation industry, hospitality, and others (4).
Considering the drastic increase in job loss with resulting hunger from financial instability and other social-economic factors resulting from lock-downs, the fall out from prolonged lockdowns to control COVID-19 will most likely be worse than the number of deaths due to COVID-19 directly.
Disclaimer: This annotation is not intended to downplay the seriousness of COVID-19. Rather it is intended to put the seriousness of the disease in context of other problems that are resulting from measures to control COVID-19.
Sources:
1) https://www.nature.com/articles/d41586-020-01181-3
3) https://www.ilo.org/global/about-the-ilo/newsroom/news/WCMS_743036/lang--en/index.htm
-
-
www.thelancet.com www.thelancet.com
-
Health, T. L. P. (2020). COVID-19 in Spain: A predictable storm? The Lancet Public Health, 0(0). https://doi.org/10.1016/S2468-2667(20)30239-5
-
-
www.thelancet.com www.thelancet.com
-
Hone, T., Mirelman, A. J., Rasella, D., Paes-Sousa, R., Barreto, M. L., Rocha, R., & Millett, C. (2019). Effect of economic recession and impact of health and social protection expenditures on adult mortality: A longitudinal analysis of 5565 Brazilian municipalities. The Lancet Global Health, 7(11), e1575–e1583. https://doi.org/10.1016/S2214-109X(19)30409-7
-
-
psyarxiv.com psyarxiv.com
-
Smith, A. M., Willroth, E. C., Gatchpazian, A., shallcross, amanda, Feinberg, M., & Ford, B. Q. (2020). Coping with Health Threats: The costs and benefits of managing emotions. [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/dn957
-
-
www.inc.com www.inc.com
-
there's a major problem with all of this instantaneous communication: It doesn't leave time to think.
-
-
twitter.com twitter.com
-
Maarten van Smeden on Twitter. (n.d.). Twitter. Retrieved October 18, 2020, from https://twitter.com/MaartenvSmeden/status/1316423658106216454
-
-
www.newscientist.com www.newscientist.com
-
Vaughan, A. (n.d.). Exclusive: Concerns raised about vital UK covid-19 infection survey. New Scientist. Retrieved October 18, 2020, from https://www.newscientist.com/article/2256942-exclusive-concerns-raised-about-vital-uk-covid-19-infection-survey/
-
-
-
50 percent effective
Take away: Cloth face masks filter approximately 50% of bacteriophage five times smaller than one SARS-CoV-2 virus. Therefore it is reasonable to assume that masks, including cloth masks, are 50% effective.
The claim: Masks are assumed to be 50% effective.
The evidence: Face masks, including home made face masks, were shown to reduce aerosol exposure (1). Masks made from various materials were shown to filter 50-68% of Bacteriophage CS2 which is 20 nm (2). When NaCl aerosols were used instead of a bacteriophage, penetration by NaCl occurred 9-98% of the time depending on the size of the particles (3). Two well written reviews detail the efficacy of facemasks (4, 5). SARS-CoV-2 virus is ~100 nm in size (6).
Sources: 1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2440799/
2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7108646/
3 https://academic.oup.com/annweh/article/54/7/789/202744
4 https://www.preprints.org/manuscript/202004.0203/v1
5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7497125/#ref23
Tags
Annotators
URL
-
-
journals.aom.org journals.aom.org
-
Daydreaming at Work Can Fuel Creativity
Summary of the article:
- We spend nearly half of each day daydreaming, and usually think that it’s a bad thing, but it turns out that highly demanding tasks make us daydream more.
- It allows us to turn off our surroundings, and can be a way of imagining solutions to the problem at hand.
- To find this out, researchers did two studies of employees and managers in South America, including mainly surveys about daydreaming.
- Daydreaming turned out to happen more when the tasks required a lot of focus - it can boost creative problem-solving as long as we’re personally invested in our work.
- However, for people who don’t identify with their work, daydreaming was linked to worse performance.
-
-
www.theguardian.com www.theguardian.com
-
Ending Covid-19 via herd immunity is “a dangerous fallacy.” (2020, October 14). The Guardian. http://www.theguardian.com/world/2020/oct/14/ending-covid-19-via-herd-immunity-is-a-dangerous-fallacy
-
-
realrisk.wintoncentre.uk realrisk.wintoncentre.ukRealRisk1
-
https://realrisk.wintoncentre.uk/. Retrieved 16-10-2020
-
-
www.coe.int www.coe.int
-
AI and control of Covid-19 coronavirus. (n.d.). Artificial Intelligence. Retrieved October 15, 2020, from https://www.coe.int/en/web/artificial-intelligence/ai-and-control-of-covid-19-coronavirus
-
-
news.sky.com news.sky.com
-
Coronavirus excess fatalities: How pandemic is impacting the lives and deaths of those who don’t have COVID. (n.d.). Sky News. Retrieved October 15, 2020, from https://news.sky.com/story/coronavirus-excess-fatalities-how-pandemic-is-impacting-the-lives-and-deaths-of-those-who-dont-have-covid-12103141
-
-
iaap-journals.onlinelibrary.wiley.com iaap-journals.onlinelibrary.wiley.com
-
Tong, K. K., Chen, J. H., Yu, E. W., & Wu, A. M. S. (n.d.). Adherence to COVID-19 Precautionary Measures: Applying the Health Belief Model and Generalised Social Beliefs to a Probability Community Sample. Applied Psychology: Health and Well-Being, n/a(n/a). https://doi.org/10.1111/aphw.12230
-
-
digitalcommons.daemen.edu digitalcommons.daemen.edu
-
Scheid, J., Lupien, S., Ford, G., & West, S. (2020). Physiological and Psychological Impact of Face Mask Usage during the COVID-19 Pandemic.
International Journal of Environmental Research and Public Health</Em>. Volume 78, Issue 18, 6655.</P>. https://doi.org/10.3390/ijerph17186655
-
-
www.emerald.com www.emerald.com
-
Lau, P. Y. F. (2020). Fighting COVID-19: Social capital and community mobilisation in Hong Kong. International Journal of Sociology and Social Policy, ahead-of-print(ahead-of-print). https://doi.org/10.1108/IJSSP-08-2020-0377
-
-
academic.oup.com academic.oup.com
-
Yang Chan, E. Y., Shahzada, T. S., Sham, T. S. T., Dubois, C., Huang, Z., Liu, S., Ho, J. Y., Hung, K. K. C., Kwok, K. O., & Shaw, R. (n.d.). Narrative review of non-pharmaceutical behavioural measures for the prevention of COVID-19 (SARS-CoV-2) based on the Health-EDRM framework. British Medical Bulletin. https://doi.org/10.1093/bmb/ldaa030
-
-
www.idunn.no www.idunn.no
-
Krumsvik, R. J. (2020). Extended Editorial. Nordic Journal of Digital Literacy, 15(03), 141–152. https://doi.org/10.18261/issn.1891-943x-2020-03-01
-
-
covid-19.iza.org covid-19.iza.org
-
Tani, M., Cheng, Z., Mendolia, S., Paloyo, A. R., & Savage, D. (2020). Working Parents, Financial Insecurity, and Child-Care: Mental Health in the Time of COVID-19. IZA Discussion Paper, 13588.
-
-
twitter.com twitter.com
-
Dr Natalie Shenker on Twitter. (n.d.). Twitter. Retrieved October 13, 2020, from https://twitter.com/DrNShenker/status/1314475759508107265
-
-
ajph.aphapublications.org ajph.aphapublications.org
-
Scherer, L. D., & Pennycook, G. (2020). Who Is Susceptible to Online Health Misinformation? American Journal of Public Health, 110(S3), S276–S277. https://doi.org/10.2105/AJPH.2020.305908
-
-
blogs.bmj.com blogs.bmj.com
-
Abraar Karan: Politics and public health in America—taking a stand for what is right. (2020, October 9). The BMJ. https://blogs.bmj.com/bmj/2020/10/09/abraar-karan-politics-and-public-health-in-america-taking-a-stand-for-what-is-right/
-
-
www.acpjournals.org www.acpjournals.org
-
In comparison, the ratio is approximately 2.5 times greater than the estimated IFR for seasonal influenza
Take away:
If correct numerators and denominators are used, COVID-19 is at least 10 times as deadly as seasonal influenza.
The claim:
The Infection Fatality Ratio for COVID-19 is “approximately 2.5 times higher than the estimated IFR for seasonal influenza.”
The evidence:
Blackburn et al. report an infection fatality ratio among community-living adults of 0.26% (1). If institutionalized adults had been included the ratio would be higher, likely approximating the 0.6% mortality rate among exposed individuals readily calculated by combining official death tolls, the known 30% undercount (2), and a definitive CDC study that found 10 times as many people have been exposed to the novel coronavirus than are reported as cases (3). Among the elderly, Blackburn et al. calculate COVID-19 is 2.5 times deadlier than seasonal flu. This is clearly an underestimate:
1) Blackburn et al. use CDC estimates of case-fatality rates calculated on the basis of all Americans, including the institutionalized, not limited to much healthier community-dwellers.
2) The seasonal influenza case fatality rates reported by the CDC, including the often cited 0.1% overall, are for symptomatic cases. Their denominators are estimated by using the reported number of influenza hospitalizations to guess the burden of clinical illness (4). But antibody studies show that 65%-85% of people infected with influenza never develop symptoms (5). The 0.6% mortality rate calculated here for SARS-CoV-2-exposed individuals is 6 times higher than the 0.1% usually cited for seasonal influenza. Given the overestimation of commonly accepted influenza mortality rates due to failure to take asymptomatic infections into account, SARS-CoV-2 can be seen to be not 2.5 times, or even 6 times, but at least 10 times as lethal as seasonal flu.
Sources:
1 http://www.acpjournals.org/doi/10.7326/M20-5352
2 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2767980
3 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2768834
4 https://www.cdc.gov/flu/about/burden/how-cdc-estimates.htm
-
-
www.reddit.com www.reddit.com
-
r/BehSciResearch—Review on combatting the COVID misinformation flood. (n.d.). Reddit. Retrieved October 12, 2020, from https://www.reddit.com/r/BehSciResearch/comments/j9mrlp/review_on_combatting_the_covid_misinformation/
-
-
www.thelancet.com www.thelancet.com
-
Kavanagh, M. M. (2020). US elections and a foreign policy for pandemics. The Lancet Public Health, 5(10), e517–e518. https://doi.org/10.1016/S2468-2667(20)30211-5
-
-
www.theguardian.com www.theguardian.com
-
Continual lockdowns are not the answer to bringing Covid under control | Devi Sridhar. (2020, October 10). The Guardian. http://www.theguardian.com/commentisfree/2020/oct/10/continual-local-lockdowns-answer-covid-control
-
-
covid-19.iza.org covid-19.iza.org
-
COVID-19 and the Labor Market. (n.d.). IZA – Institute of Labor Economics. Retrieved October 11, 2020, from https://covid-19.iza.org/publications/dp13749/
-
-
covid-19.iza.org covid-19.iza.org
-
COVID-19 and the Labor Market. (n.d.). IZA – Institute of Labor Economics. Retrieved October 11, 2020, from https://covid-19.iza.org/publications/dp13753/
-
-
covid-19.iza.org covid-19.iza.org
-
COVID-19 and the Labor Market. (n.d.). IZA – Institute of Labor Economics. Retrieved October 10, 2020, from https://covid-19.iza.org/publications/dp13569/
-
-
www.ecdc.europa.eu www.ecdc.europa.eu
-
New tool for the early detection of public health threats from Twitter data: Epitweetr. (2020, October 1). European Centre for Disease Prevention and Control. https://www.ecdc.europa.eu/en/news-events/new-tool-early-detection-public-health-threats-twitter-data-epitweetr
-
-
www.theguardian.com www.theguardian.com
-
correspondent, N. D. S. (2020, October 9). “Brain fog”: The people struggling to think clearly months after Covid. The Guardian. https://www.theguardian.com/world/2020/oct/09/brain-fog-the-people-struggling-to-think-clearly-months-after-covid
-
-
twitter.com twitter.com
-
Adam Kucharski on Twitter. (n.d.). Twitter. Retrieved October 10, 2020, from https://twitter.com/AdamJKucharski/status/1313760847932596224
-
-
www.psychologs.com www.psychologs.com
-
Covid-19: Is Behavioural Science The Key To Handle The Pandemic? (n.d.). Retrieved October 10, 2020, from https://www.psychologs.com/article/covid-19-is-behavioral-science-the-key-to-handle-the-pandemic
-
-
www.bloomberg.com www.bloomberg.com
-
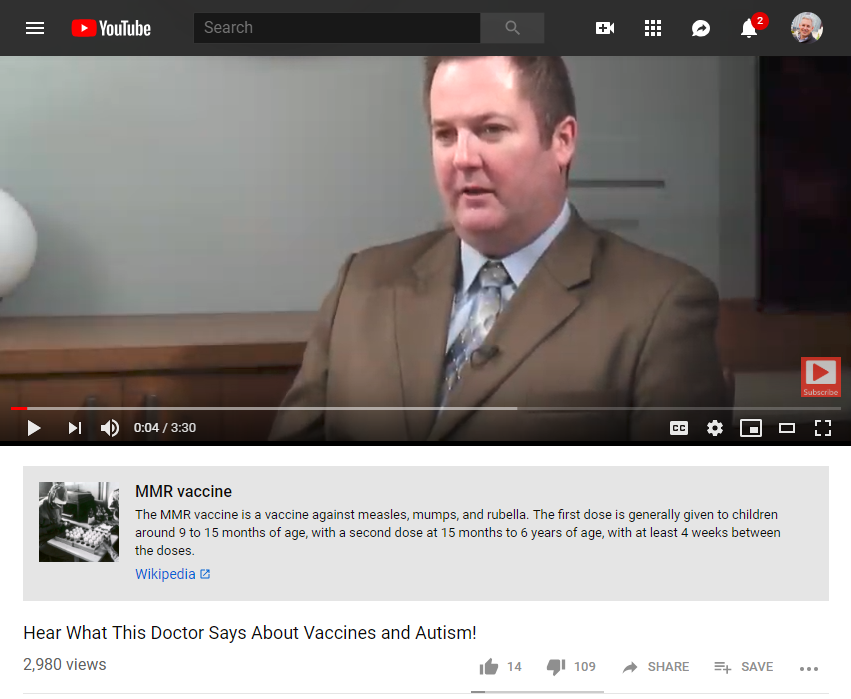
A 2015 clip about vaccination from iHealthTube.com, a “natural health” YouTube channel, is one of the videos that now sports a small gray box.
Does this box appear on the video itself? Apparently not...
Examples:
But nothing on the embedded version:
A screengrab of what this looks like:
-
-
www.nytimes.com www.nytimes.com
-
A 2016 Lancet study found that universal breast-feeding would prevent 800,000 child deaths a year across the globe and yield $300 billion in savings from reduced health care costs and improved economic outcomes for those reared on breast milk.
Pure corruption here. Protectionism to prop up profits of approximately 630 million versus major benefits and savings of 300 billion. Even if you look at the calculus of the entire industry of 70 billion it becomes a no brainer.
-
-
www.nytimes.com www.nytimes.com
-
She reached behind her to her bookshelf, which held about a dozen blue bottles of something called Real Water, which is not stripped of “valuable electrons,” which supposedly creates free radicals something something from the body’s cells.
I question her credibility to market claims like this. I suspect she has no staff scientist or people with the sort of background to make such claims. Even snake oil salesmen like Dr. Oz are pointedly putting us in hands way too make a buck.
-
-
blogs.scientificamerican.com blogs.scientificamerican.com
-
Bad economic times could lead to deaths of people with low income who are most vulnerable to an economic downturn.
This is the most likely place that governments and the richer ruling elites are likely to fail their societies. Even the United States is like to do this and one need look no further than their response to the hurricane aftermath in Puerto Rico to see this.
-
-
www.economist.com www.economist.com
-
many Indians continue to defecate in the open. Bangladesh’s government and charities have built latrines, too, but they have worked harder to stigmatise open defecation. Often they install latrines for the poor and then prod richer folk into following their example. A new, surprising, finding is that this works better than expecting people to copy their social superiors.
-
Many lives have been saved by parents doing something simple. Beginning in the 1960s American military doctors and researchers in Dhaka developed a therapy for acute diarrhoea—a sweet, salty oral rehydration solution. This is now dirt cheap and widely available. At the last count, fully 84% of Bangladeshi parents with stricken children fed it to them (only a third saw a doctor). Thinly populated African countries are struggling to match that. One promising idea is to distribute the sachets along with Coca-Cola—which gets everywhere.
amazing the reach of Coca-Cola!
-
-
www.theatlantic.com www.theatlantic.com
-
To find a cure for what ails America, Chetty will need to understand all of this wild variation. Which factors foster opportunity, and which impede it? The next step will be to find local interventions that can address these factors—and to prove, with experimental trials, that the interventions work
I suspect that racial inequalities like Redlining, school support, and public housing issues (including evictions and predatory lending) will overlay these unmobile areas. cf Scarlet E series from On the Media.
-
-
parenting.nytimes.com parenting.nytimes.com
-
How this phenomenon translates into absolute, rather than relative, risk, however, is a bit thorny. A large study published in 2018, for instance, found that among women who had children between 34 and 47, 2.2 percent developed breast cancer within three to seven years after they gave birth (among women who never had children, the rate was 1.9 percent). Over all, according to the American Cancer Society, women between 40 and 49 have a 1.5 percent chance of developing breast cancer.
The rates here are so low as to be nearly negligible on their face. Why bother reporting it?
-
-
www.theatlantic.com www.theatlantic.com
-
They’re mostly things that everyone was supposed to be doing all along, such as ensuring that bathrooms have exhaust fans and that air filters are changed regularly and of high-enough quality to catch the virus. That means they should be high-efficiency particulate air (HEPA) filters or MERV-rated 13 or 14, which are essentially the N-95 masks of air filters.
-
During the SARS coronavirus outbreak, in 2003, a cluster of cases in Hong Kong was attributed to one person with diarrhea in a poorly ventilated apartment building.
toilet plume, two words everyone just loves!
-
-
collect.readwriterespond.com collect.readwriterespond.com
-
This a harrowing story made even sadder by the grim reality of the statistics.
I'm almost losing count of how many racial health disparity stories I've been seeing lately. It's so common I've got tags for it on my site now.
-
-
www.nytimes.com www.nytimes.com
-
“We ought to have a social compact: If you’re sick, whether you’ve got Covid-19 or not, you should separate yourself from society,” Mr. Gostin said. “That’s your part of the bargain, you’re doing it for your neighbors, your family and your community.”“In exchange,” he said, “we as a nation owe you the right to a humane period of separation, where we meet your essential needs like medicine, health care, food and sick pay.”
-
-
hybridpedagogy.org hybridpedagogy.org
-
Reporting on a study at Queensborough Community College, also in the CUNY system, Sheila Beck notes that the library’s reserve textbook collection is “heavily used,” however, staffing and other concerns have prompted librarians to consider “less labor intensive and less costly alternatives.“ Beyond textbook reserves, academic librarians can help students to locate required course readings in other ways: older editions of their required textbook, pre- or post-prints of articles in institutional repositories, articles or other texts in databases subscribed to by the library, or readings that may be in the public domain or otherwise available on the open web.
The basic economics of this system would indicate (especially as classes become larger and larger) that more careful consideration of choice, economics, accessibility, availability, etc. on a larger institutional level creates larger marginal gains for those in the class. If a staff librarian, teacher, or someone else within the system does the leg-work up front and does it well, then the dozens or even hundreds of students in the course don't need to spend (read: waste) their own time re-inventing the proverbial textbook wheel once they're in the class.
Portions of the situation here make me wonder if we might pull a page from Dr. Peter Pronovost's playbook in the health care space and create a simple checklist of what to do when planning for textbooks and readings. Checklists that include things like:
- will the texts actually be used?
- will they be primary to the subject or are they supplementary?
- What are their prices?
- Are alternate materials available?
- Are older editions available?
- are public domain or open web versions available?
- are there copies in the library? reserves? pirated versions? pre/post prints?
- etc.
Once such a checklist is available, institutions should require that it be available along with syllabi and other course listings.
cross references:
-
-
www.rt.com www.rt.com
-
A scientific review of the science behind lockdown concludes the policy was a MISTAKE & will have caused MORE deaths from Covid-19
Take Away: The new scientific paper confirms earlier modeling work and should not be interpreted as a detailed prediction for future deaths due to the ongoing pandemic.
The Claim: "A scientific review of the science behind lockdown concludes the policy was a MISTAKE & will have caused MORE deaths from Covid-19"
The Evidence: The scientific process involves replication and confirmation of experiments and studies. A new paper replicates and expands on an early modeling study of the COVID-19 pandemic in England (1). Their findings support the earlier results. However, there are limitations to the replication paper, which does not accurately reflect the current state of the pandemic response and does not make detailed predictions for a second wave of infections and deaths.
A recent expert response to the paper further explains (2):
"It needs to be stressed that all the simulations assume that interventions are only in place for 3 months (18th April – 18th July) and then completely relaxed. This gives rise to a strange set of scenarios where a second wave is allowed to progress in an uncontrolled manner."
“It is this that leads to the counter-intuitive headline finding “that school closures would result in more overall covid-19 deaths than no school closures” – actually what the authors find is that a short period of intense lock-down (including the closure of schools) leads to a large second wave if it is allowed to run with no controls. To be fair the authors do highlight this in the paper, but it is not in the reported press release." -Prof Matt Keeling, Professor of Populations and Disease, University of Warwick
Sources:
-
-
www.bmj.com www.bmj.com
-
The model predicted that school closures and isolation of younger people would increase the total number of deaths, albeit postponed to a second and subsequent waves. The findings of this study suggest that prompt interventions were shown to be highly effective at reducing peak demand for intensive care unit (ICU) beds but also prolong the epidemic, in some cases resulting in more deaths long term. This happens because covid-19 related mortality is highly skewed towards older age groups. In the absence of an effective vaccination programme, none of the proposed mitigation strategies in the UK would reduce the predicted total number of deaths below 200 000.
Take away: This model excludes the possibility of vaccination. As many vaccines are in stage three clinical trials, the conclusion that more people will die from closing schools, etc. will most likely not be realized.
The claim: School closures and isolation of younger people will increase total number of deaths from second and subsequent waves of COVID-19 when restrictions are lifted.
The evidence: This model predicts more deaths from the combination of place closures such as schools, case isolations, household quarantine, and social distancing of over 70s than for the combination of case isolation, household quarantine, and social distancing for over 70s. The majority of the deaths for the combination of place closures, case isolations, household quarantine, and social distancing of over 70s occur once the restrictions are lifted. This model excludes the possibility of a vaccine reducing the size of the second wave.
At least ten companies have a COVID-19 vaccine in the final stage (Phase III) of clinical trials (1). Therefore a model which excludes vaccination will most likely not be accurate to reality once a vaccine is widely administered.
Source:
1 https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
-
-
twitter.com twitter.com
-
Shauna Brail on Twitter. (n.d.). Twitter. Retrieved October 9, 2020, from https://twitter.com/shaunabrail/status/1313818873163067392
-
-
www.thelancet.com www.thelancet.com
-
Horton, R. (2020). Offline:Reasons for hope. Lancet, 396
-
-
www.politico.com www.politico.com
-
CDC reverses course on testing for asymptomatic people who had Covid-19 contact
Take Away
Transmission of viable SARS-CoV-2 RNA can occur even from an infected but asymptomatic individual. Some people never become symptomatic. That group usually becomes non-infectious after 14 days from initial infection. For persons displaying symptoms , the SARS-CoV-2 RNA can be detected for 1 to 2 days prior to symptomatology. (1)
The Claim
Asymptomatic people who had SARS-CoV-2 contact should be tested.
The Evidence
Yes, this is a reversal of August 2020 advice. What is the importance of asymptomatic testing?
Studies show that asymptomatic individuals have infected others prior to displaying symptoms. (1)
According to the CDC’s September 10th 2020 update approximately 40% of infected Americans are asymptomatic at time of testing. Those persons are still contagious and are estimated to have already transmitted the virus to some of their close contacts. (2)
In a report appearing in the July 2020 Journal of Medical Virology, 15.6% of SARS-CoV-2 positive patients in China are asymptomatic at time of testing. (3)
Asymptomatic infection also varies by age group as older persons often have more comorbidities causing them to be susceptible to displaying symptoms earlier. A larger percentage of children remain asymptomatic but are still able to transmit the virus to their contacts. (1) (3)
Transmission modes
Droplet transmission is the primary proven mode of transmission of the SARS-CoV-2 virus, although it is believed that touching a contaminated surface then touching mucous membranes, for example, the mouth and nose can also serve to transmit the virus. (1)
It is still unclear how big or small a dose of exposure to viable viral particles is needed for transmission; more research is needed to elucidate this. (1)
Citations
(1) https://www.who.int/news- room/commentaries/detail/transmission-of-sars-cov-2- implications-for-infection-prevention-precautions
(2) https://www.cdc.gov/coronavirus/2019- ncov/hcp/planning-scenarios.html
(3) He J, Guo Y, Mao R, Zhang J. Proportion of asymptomatic coronavirus disease 2019: A systematic review and metaanalysis. J Med Virol. 2020;1– 11.https://doi.org/10.1002/jmv.26326
-
-
www.thelancet.com www.thelancet.com
-
Bozorgmehr, K. (2020). Power of and power over COVID-19 response guidelines. The Lancet, 0(0). https://doi.org/10.1016/S0140-6736(20)32081-X
-
-
trailrunnermag.com trailrunnermag.com
-
Multiply that number by 85 percent to roughly approximate an effort cap for easy runs (though adjusting to a different percentage if you feel like that’s a bit too hard or too easy).
Another article suggests subtracting 20bpm
-
-
videocast.nih.gov videocast.nih.gov
-
NIH VideoCast—Joseph Leiter NLM/MLA Lectureship: Digital Epidemiology and the COVID-19 Pandemic. (n.d.). Retrieved 6 October 2020, from https://videocast.nih.gov/watch=38269
-
-
www.theguardian.com www.theguardian.com
-
Queen stresses need for trusted news sources during Covid crisis. (2020, October 4). The Guardian. http://www.theguardian.com/media/2020/oct/05/queen-elizabeth-stresses-need-for-trusted-news-sources-during-covid-crisis
-
-
covid-19.iza.org covid-19.iza.org
-
IZA – Institute of Labor Economics. ‘COVID-19 and the Labor Market’. Accessed 6 October 2020. https://covid-19.iza.org/publications/dp13742/.
-
-
covid-19.iza.org covid-19.iza.org
-
IZA – Institute of Labor Economics. ‘COVID-19 and the Labor Market’. Accessed 6 October 2020. https://covid-19.iza.org/publications/dp13715/.
-
-
covid-19.iza.org covid-19.iza.org
-
IZA – Institute of Labor Economics. ‘COVID-19 and the Labor Market’. Accessed 6 October 2020. https://covid-19.iza.org/publications/dp13707/.
-
-
covid-19.iza.org covid-19.iza.org
-
IZA – Institute of Labor Economics. ‘COVID-19 and the Labor Market’. Accessed 6 October 2020. https://covid-19.iza.org/publications/dp13683/.
-
-
covid-19.iza.org covid-19.iza.org
-
IZA – Institute of Labor Economics. ‘COVID-19 and the Labor Market’. Accessed 6 October 2020. https://covid-19.iza.org/publications/dp13670/.
-
-
covid-19.iza.org covid-19.iza.org
-
IZA – Institute of Labor Economics. ‘COVID-19 and the Labor Market’. Accessed 6 October 2020. https://covid-19.iza.org/publications/dp13648/.
-
-
www.statnews.com www.statnews.com
-
Long after a Covid-19 infection, mental and neurological effects smolder. (2020, August 12). STAT. https://www.statnews.com/2020/08/12/after-covid19-mental-neurological-effects-smolder/
-
-
alama.org.uk alama.org.uk
-
Covid-19 Medical Risk Assessment – Alama. (n.d.). Retrieved October 2, 2020, from https://alama.org.uk/covid-19-medical-risk-assessment/
-
-
psyarxiv.com psyarxiv.com
-
Low, Rachel S. T., Nickola Overall, Valerie Chang, and Annette M. E. Henderson. ‘Emotion Regulation and Psychological and Physical Health during a Nationwide COVID-19 Lockdown’, 1 October 2020. https://doi.org/10.31234/osf.io/pkncy.
-
-
psyarxiv.com psyarxiv.com
-
Omary, Areen. ‘COVID-19 Health Status Scale (CHSS)’. Preprint. PsyArXiv, 30 September 2020. https://doi.org/10.31234/osf.io/2wnxd.
-
-
www.thelancet.com www.thelancet.com
-
Franco-Paredes, Carlos, Nazgol Ghandnoosh, Hassan Latif, Martin Krsak, Andres F. Henao-Martinez, Megan Robins, Lilian Vargas Barahona, and Eric M. Poeschla. ‘Decarceration and Community Re-Entry in the COVID-19 Era’. The Lancet Infectious Diseases 0, no. 0 (29 September 2020). https://doi.org/10.1016/S1473-3099(20)30730-1.
-
-
journals-sagepub-com.access.library.unisa.edu.au journals-sagepub-com.access.library.unisa.edu.au
-
Forexample, there is evidence that people inhigher socio-economic groups are morelikely to be successful in quitting smoking
Privilege impacts the ability to make important health decisions
-
-
psyarxiv.com psyarxiv.com
-
MacFarlane, Douglas, Li Qian Tay, Mark J. Hurlstone, and Ullrich Ecker. ‘Refuting Spurious COVID-19 Treatment Claims Reduces Demand and Misinformation Sharing’, 30 September 2020. https://doi.org/10.31234/osf.io/q3mkd.
-
-
www.medrxiv.org www.medrxiv.org
-
Kaplan, Edward H, Dennis Wang, Mike Wang, Amyn A Malik, Alessandro Zulli, and Jordan H Peccia. ‘Aligning SARS-CoV-2 Indicators via an Epidemic Model: Application to Hospital Admissions and RNA Detection in Sewage Sludge’. Preprint. Infectious Diseases (except HIV/AIDS), 29 June 2020. https://doi.org/10.1101/2020.06.27.20141739.
-
- Sep 2020
-
twitter.com twitter.com
-
Carl Heneghan on Twitter. (n.d.). Twitter. Retrieved September 30, 2020, from https://twitter.com/carlheneghan/status/1309905734403002369
-
-
www.youtube.com www.youtube.com
-
Petrie-Flom Center
COVID-19 and the Politics of Reproductive Health: Global Perspectives. (2020, August 18). https://www.youtube.com/watch?v=Kex9O_cwMwo
-
-
www.thelancet.com www.thelancet.com
-
Wilkinson, Jack, Kellyn F. Arnold, Eleanor J. Murray, Maarten van Smeden, Kareem Carr, Rachel Sippy, Marc de Kamps, et al. ‘Time to Reality Check the Promises of Machine Learning-Powered Precision Medicine’. The Lancet Digital Health 0, no. 0 (16 September 2020). https://doi.org/10.1016/S2589-7500(20)30200-4.
Tags
- is:report
- electronic health database
- collaboration
- lang:en
- machine learning powered precision medicine
- personalised medical approach
- algorithmic complexity
- revolution
- challenges
- clinical practice
- improved diagnosis
- prediction of individual responses
- clinical science
- machine learning
Annotators
URL
-
-
www.thelancet.com www.thelancet.com
-
Torres, Irene, Osvaldo Artaza, Barbara Profeta, Cristina Alonso, and JaHyun Kang. ‘COVID-19 Vaccination: Returning to WHO’s Health For All’. The Lancet Global Health 0, no. 0 (25 September 2020). https://doi.org/10.1016/S2214-109X(20)30415-0.
-
-
www.nature.com www.nature.com
-
Krammer, Florian. ‘SARS-CoV-2 Vaccines in Development’. Nature, 23 September 2020, 1–16. https://doi.org/10.1038/s41586-020-2798-3.
-
-
www.bbc.co.uk www.bbc.co.uk
-
Covid: Cardiff and Swansea go into local lockdown—BBC News. (n.d.). Retrieved September 29, 2020, from https://www.bbc.co.uk/news/uk-wales-54310400
-
-
www.youtube.com www.youtube.com
-
Learning lessons before launching an inquiry—IfG LIVE 2020 Labour Fringe Programme—YouTube. (n.d.). Retrieved September 29, 2020, from https://www.youtube.com/watch?v=cCZl-naQ6UM
-
-
www.scientificamerican.com www.scientificamerican.com
-
The COVID-19 Pandemic Is Changing Our Dreams—Scientific American. (n.d.). Retrieved September 29, 2020, from https://www.scientificamerican.com/article/the-covid-19-pandemic-is-changing-our-dreams/
-
-
archive.theincline.com archive.theincline.com
-
psyarxiv.com psyarxiv.com
-
Garrett, P. M., White, J. P., Lewandowsky, S., Kashima, Y., Perfors, A., Little, D. R., Geard, N., Mitchell, L., Tomko, M., & Dennis, S. (2020). The acceptability and uptake of smartphone tracking for COVID-19 in Australia [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/7tme6
-
-
www-sciencedirect-com.ezproxy.neu.edu www-sciencedirect-com.ezproxy.neu.edu
-
The impact of global warming on population health is a growing concern. Solar energy workers often work in very hot weather; where OSHA supports that there exist some hazards attempting to the health and safety of the workforce. Among the heat-related effects defined as a consequence of exposures to hot environments are, dehydration, heat exhaustion, heat stroke, and death. In order to ensure the safety of the solar workforce, the present study aims to provide with relevant information that could contribute to the development or improvement of safety procedures.The research paper briefly outlines the relation between sunny environments, heat load, heat-related occupational and safety, natural hazards, and climate change conditions. Followed by the description of the assessment method and safety limits. The assessment of levels of heat stress was based on a
direct relation of results to health (not necessarily worker productivity however)
-
-
www.theguardian.com www.theguardian.com
-
Brooks, L., & Adams, R. (2020, September 24). Hundreds of thousands of students in Scotland banned from socialising. The Guardian. https://www.theguardian.com/education/2020/sep/24/thousands-of-students-in-isolation-at-20-uk-universities
-
-
twitter.com twitter.com
-
Manic pixie dream gàidheal✨ on Twitter. (n.d.). Twitter. Retrieved September 28, 2020, from https://twitter.com/nicmharcuis/status/1309599281280679941
-
-
www.fda.gov www.fda.gov
-
Commissioner, O. of the. (2020, September 23). Coronavirus (COVID-19) Update: FDA Authorizes First Point-of-Care Antibody Test for COVID-19. FDA; FDA. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-first-point-care-antibody-test-covid-19
Tags
- public health response
- lang:en
- COVID-19
- is:webpage
- serology
- antibody test
- is:news
- protection
- blood sample
- FDA
- strategy
- point-of-care
Annotators
URL
-
-
www.thelancet.com www.thelancet.com
-
Knawy, B. A., Adil, M., Crooks, G., Rhee, K., Bates, D., Jokhdar, H., Klag, M., Lee, U., Mokdad, A. H., Schaper, L., Hazme, R. A., Khathaami, A. M. A., & Abduljawad, J. (2020). The Riyadh Declaration: The role of digital health in fighting pandemics. The Lancet, 0(0). https://doi.org/10.1016/S0140-6736(20)31978-4
-
-
www.thelancet.com www.thelancet.com
-
Williams, R., Jenkins, D. A., Ashcroft, D. M., Brown, B., Campbell, S., Carr, M. J., Cheraghi-sohi, S., Kapur, N., Thomas, O., Webb, R. T., & Peek, N. (2020). Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: A retrospective cohort study. The Lancet Public Health, 0(0). https://doi.org/10.1016/S2468-2667(20)30201-2
-
-
blog.petrieflom.law.harvard.edu blog.petrieflom.law.harvard.edu
-
Who’s to Blame for COVID-19 Outbreaks at Colleges and Universities? (2020, September 15). Bill of Health. http://blog.petrieflom.law.harvard.edu/2020/09/15/whos-to-blame-for-covid-19-outbreaks-at-colleges-and-universities/
Tags
- college
- transmission
- lang:en
- COVID-19
- law
- university
- public health intervention
- responsibility
- administration
- is:blog
- safety
- outbreak
- blame
- USA
Annotators
URL
-
-
psyarxiv.com psyarxiv.com
-
Tillman, G. (2020). Disordered Social Media Use and Fear of COVID-19 and the Association with Stress and Depression. https://doi.org/10.31234/osf.io/dbg62
-
-
www.huffpost.com www.huffpost.com
-
HuffPost UK. ‘The Coronavirus Is Creating A Mental Health Crisis For Health Care Workers’, 21 September 2020. https://www.huffpost.com/entry/health-care-workers-covid-mental-health_n_5f625a6ac5b6c6317cfed815.
-
-
www.bbc.co.uk www.bbc.co.uk
-
Triggle, Nick. ‘Is It Time We Learned to Live with the Virus?’ BBC News, 21 September 2020, sec. Health. https://www.bbc.com/news/health-54228649.
-
-
www.nature.com www.nature.com
-
Leask, Julie. ‘Vaccines — Lessons from Three Centuries of Protest’. Nature 585, no. 7826 (21 September 2020): 499–501. https://doi.org/10.1038/d41586-020-02671-0.
-
-
www.huffingtonpost.co.uk www.huffingtonpost.co.uk
-
HuffPost UK. ‘Exclusive: Public Want Test And Trace Taken Out Of Hands Of Private Firms’, 21 September 2020. https://www.huffingtonpost.co.uk/entry/exclusive-public-want-track-and-trace-taken-off-serco_uk_5f6785ecc5b6480e8970b968.
-
-
psyarxiv.com psyarxiv.com
-
Lange, Ann-Marie G de, Tobias Kaufmann, Daniel S Quintana, Adriano Winterton, Lars T. Westlye, and Klaus P. Ebmeier. ‘Risk Factors Associated with Loneliness, Social Isolation, and Neuroticism in the UK Biobank Cohort’. Preprint. PsyArXiv, 21 September 2020. https://doi.org/10.31234/osf.io/q8kjv.
Tags
- depression
- UK
- risk factor
- neuroticism
- social deprivation
- vulnerable
- social isolation
- public health
- loneliness
- unhealthy lifestyle
- mental health
- comorbidities
- physical health
- lang:en
- COVID-19
- United Kingdom
- aging
- social health
- Biobank
- socioeconomic conditions
- is:preprint
- cardiovascular risk
Annotators
URL
-
-
oneheglobal.org oneheglobal.org
-
Most instructors will have the experience and knowledge of their students’ situation to make wise choices about activities that will work best.
Academic professors are acknowledging their students well-being which is important and shows care from both sides of the professor and student. This allows the student know that even though the professor is mainly involved with education, they still care.
-
-
www.independent.co.uk www.independent.co.uk
-
Hospitals told not to test staff or patients for Covid-19. (2020, September 18). The Independent. https://www.independent.co.uk/news/health/coronavirus-nhs-testing-hospitals-shortage-b485589.html
-
-
-
Anderson-Carpenter, K., & Neal, Z. (2020). Racial Disparities in COVID-19 Impacts in Michigan, USA. 10.31234/osf.io/st2rp
-
-
psyarxiv.com psyarxiv.com
-
Mactavish, A., Mastronardi, C., Menna, R., Babb, K. A., Battaglia, M., Amstadter, A. B., Rappaport, L. (2020). The Acute Impact of the COVID-19 Pandemic on Children’s Mental Health in Southwestern Ontario. 10.31234/osf.io/5cwb4
-
-
advances.sciencemag.org advances.sciencemag.org
-
Holman, E. A., Thompson, R. R., Garfin, D. R., & Silver, R. C. (2020). The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the U.S. Science Advances, eabd5390. https://doi.org/10.1126/sciadv.abd5390
-
-
psyarxiv.com psyarxiv.com
-
Sueki, H., & Ueda, M. (2020). Short-term effect of the COVID-19 pandemic on suicidal ideation: A prospective cohort study. https://doi.org/10.31234/osf.io/3jevh
-
-
www.ncbi.nlm.nih.gov www.ncbi.nlm.nih.gov
-
There are two possible approaches to build widespread SARS-CoV-2 immunity: (1) a mass vaccination campaign, which requires the development of an effective and safe vaccine, or (2) natural immunization of global populations with the virus over time. However, the consequences of the latter are serious and far-reaching—a large fraction of the human population would need to become infected with the virus, and millions would succumb to it.
Take away: Mass infection without vaccination to achieve herd immunity will result in millions of deaths based on the observed death rate and may not result in herd immunity due to virus mutation. Historically, vaccination results in less deaths than the disease.
The claim: Herd immunity from widespread disease instead of vaccination will lead to many people dying.
The evidence: Approximately 50-67% of a given population is estimated to need to be infected for herd immunity to COVID-19 to exist which will result in millions of deaths. This is supported by additional publications (1, 2). This number assumes that the virus will not mutate to the point where re-infection is possible. If mutation occurs, COVID could become established in the general population similar to influenza or the common cold (3). A third publication estimates a needed infected percentage of 29-74% (4). These publications support the statement that millions will die if herd immunity is achieved via infection without vaccination. Historically, vaccination results in fewer deaths/disease on a population level than the disease for which the vaccine is designed to prevent (5-7).
Sources:
1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7314002/
2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262166/pdf/JMV-9999-na.pdf
3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7164482/
5 https://pubmed.ncbi.nlm.nih.gov/28708957/
-
-
www.uni-konstanz.de www.uni-konstanz.de
-
Ten minutes of massage or rest will help your body fight stress
- Short-term treatments like a massage, or just resting for a bit, reduce stress by boosting the parasympathetic nervous system (PNS).
- Relaxation therapies show promise as a way to treat stress, but so far scientists haven’t developed a standardised method to test them - until now.
- This study is the first standardised approach, and the results show that both rest and a massage increase heart rate variability (HRV) - higher HRV = greater relaxation.
- Researchers say this shows we don’t need professional treatment in order to relax, even a 10-minute rest can boost our PNS and calm us down.
- These conclusions will enable further experiments to study how different relaxation methods can help people with stress-related conditions like depression
-
-
www.nature.com www.nature.com
-
Lincoln, M. (2020). Study the role of hubris in nations’ COVID-19 response. Nature, 585(7825), 325–325. https://doi.org/10.1038/d41586-020-02596-8
-
-
-
Gallagher, R. J., Doroshenko, L., Shugars, S., Lazer, D., & Welles, B. F. (2020). Sustained Online Amplification of COVID-19 Elites in the United States. ArXiv:2009.07255 [Physics]. http://arxiv.org/abs/2009.07255
-
-
www.bbc.co.uk www.bbc.co.uk
-
BBC News (2020) Vulnerable children will 'slip out of view', commissioner warns. Retrieved from: https://www.bbc.co.uk/news/uk-england-54159977
-
-
psyarxiv.com psyarxiv.com
-
Racine, S. E., Miller, A. E., Mehak, A., & Trolio, V. (2020, September 14). Examining Risk and Protective Factors for Psychological Health during the COVID-19 Pandemic. https://doi.org/10.31234/osf.io/ys8fn
-
-
elemental.medium.com elemental.medium.com
-
Austin S. (2020) This Lawyer Ran Errands for His High-Risk Wife. Then an Epidemiologist Rated His Every Move.https://elemental.medium.com/this-lawyer-ran-errands-for-his-high-risk-wife-then-an-epidemiologist-rated-his-every-move-f9a926ad96ec
-
-
psyarxiv.com psyarxiv.com
-
Kubo, T., Sugawara, D., & Masuyama, A. (2020). The effect of ego-resiliency and COVID-19-related stress on mental health among the Japanese population. https://doi.org/10.31234/osf.io/up6c3
-
-
www.dailymail.co.uk www.dailymail.co.uk
-
Take away: People are infectious for only part of the time they test positive. The tests for COVID-19 were granted emergency status by the FDA so some debate concerning the most ideal number of cycles is to be expected. It is worth noting that the FDA has the disclaimer "Negative results do not preclude 2019-nCoV infection and should not be used as the sole basis for treatment or other patient management decisions. Negative results must be combined with clinical observations, patient history, and epidemiological information (2)."
The claim: Up to 90 percent of people diagnosed with coronavirus may not be carrying enough of it to infect anyone else
The evidence: Per Walsh et al. (1), SARS-CoV-2 virus (COVID-19) is most likely infectious if the number of PCR cycles is <24 and the symptom onset to test is <8 days. RT-PCR detects the RNA, not the infectious virus. Therefore, setting the cycle threshold at 37-40 cycles will most likely result in detecting some samples with virus which is not infectious. As the PCR tests were granted emergency use by the FDA (samples include 2-9), it is not surprising that some debate exists currently about where the cycle threshold should be. Thresholds need to be set and validated for dozens of PCR tests currently in use. If identifying only infectious individuals is the goal, a lower cycle number may be justified. If detection of as many cases as possible to get closer to the most accurate death rate is the goal, setting the cycle threshold at 37-40 makes sense. A lower threshold will result in fewer COVID-19 positive samples being identified. It is worth noting that the emergency use approval granted by the FDA includes the disclaimer that a negative test does not guarantee that a person is not infected with COVID-19. RNA degrades easily. If samples are not kept cold or properly processed, the virus can degrade and result in a false negative result.
Source: 1 https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa638/5842165
2 https://www.fda.gov/media/134922/download
3 https://www.fda.gov/media/138150/download
4 https://www.fda.gov/media/137120/download
5 https://www.fda.gov/media/136231/download
6 https://www.fda.gov/media/136472/download
7 https://www.fda.gov/media/139279/download
-
-
www.politico.com www.politico.com
-
Trump officials interfered with CDC reports on Covid-19. (n.d.). POLITICO. Retrieved September 14, 2020, from https://www.politico.com/news/2020/09/11/exclusive-trump-officials-interfered-with-cdc-reports-on-covid-19-412809
-
-
www.theguardian.com www.theguardian.com
-
Coronavirus cases are rising again in the UK. Here’s what should happen next | Devi Sridhar. (2020, September 8). The Guardian. http://www.theguardian.com/commentisfree/2020/sep/08/coronavirus-cases-rising-uk-second-wave
-
-
-
Joyce, K. M., Cameron, E. E., Sulymka, J., Protudjer, J., & Roos, L. E. (2020). Changes in Maternal Substance Use During the COVID-19 Pandemic [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/htny8
-
-
psyarxiv.com psyarxiv.com
-
Rogers, S., & Cruickshank, T. (2020). Change in mental health during highly restrictive lockdown in the COVID-19 pandemic: Evidence from Australia. https://doi.org/10.31234/osf.io/zutav
-
-
psyarxiv.com psyarxiv.com
-
Rajkumar, R. P. (2020). Novel Coronavirus Disease (COVID-19) and Suicide: Conceptual and Practical Considerations [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/z7drs
-
-
-
Postdocs in crisis: Science cannot risk losing the next generation. (2020). Nature, 585(7824), 160–160. https://doi.org/10.1038/d41586-020-02541-9
-
-
www.itv.com www.itv.com
-
Peston, R. (2020, September 7). SAGE scientist warns coronavirus cases “increasing exponentially.” ITV News. https://www.itv.com/news/2020-09-07/exclusive-sage-scientist-tells-peston-coronavirus-cases-increasing-exponentially
-
-
-
Thread, C. (2020, June 19). Trolls and Tribulations: Social Media and Public Health. Medium. https://medium.com/@gocommonthread/trolls-and-tribulations-social-media-and-public-health-499bf5c8727c
-
-
papers.ssrn.com papers.ssrn.com
-
Casoria, F., Galeotti, F., & Villeval, M. C. (2020). Perceived Social Norm and Behavior Quickly Adjusted to Legal Changes During the COVID-19 Pandemic (SSRN Scholarly Paper ID 3681204). Social Science Research Network. https://doi.org/10.2139/ssrn.3681204
-
-
www.medrxiv.org www.medrxiv.org
-
Team, I. C.-19 F., & Hay, S. I. (2020). COVID-19 scenarios for the United States. MedRxiv, 2020.07.12.20151191. https://doi.org/10.1101/2020.07.12.20151191
-
-
twitter.com twitter.com
-
Johan Hellström on Twitter. (n.d.). Twitter. Retrieved September 7, 2020, from https://twitter.com/jhnhellstrom/status/1301073768748593153
-
-
www.independent.co.uk www.independent.co.uk
-
‘7,000 Health Workers Have Died of Covid-19 around World, Amnesty Says’. Accessed 7 September 2020. https://www.independent.co.uk/news/world/coronavirus-amnesty-international-healthcare-worker-deaths-uk-usa-mexico-a9704266.html.
-
-
psyarxiv.com psyarxiv.com
-
Lewandowsky, Stephan, Simon Dennis, Amy Perfors, Yoshihisa Kashima, Joshua White, Paul Michael Garrett, Daniel R. Little, and Muhsin Yesilada. ‘Public Acceptance of Privacy-Encroaching Policies to Address the COVID-19 Pandemic in the United Kingdom’. Preprint. PsyArXiv, 4 September 2020. https://doi.org/10.31234/osf.io/njwmp.
Tags
- widespread acceptance
- UK
- co-location tracking
- public acceptance
- time limited
- infected
- social distancing
- tracking technology
- public
- lang:en
- COVID-19
- contact
- United Kingdom
- willingness
- immunity passport
- health agencies
- privacy-encroaching policy
- opt-out clause
- antibodies
- is:preprint
Annotators
URL
-
-
psyarxiv.com psyarxiv.com
-
Paudel, Dhirendra. ‘ABC Framework of Fear of COVID-19 for Psychotherapeutic Intervention in Nepal: A Review’. Preprint. PsyArXiv, 4 September 2020. https://doi.org/10.31234/osf.io/9sj4a.
-
-
psyarxiv.com psyarxiv.com
-
Lee, Hyeon-seung, Derek Dean, Tatiana Baxter, Taylor Griffith, and Sohee Park. ‘Deterioration of Mental Health despite Successful Control of the COVID-19 Pandemic in South Korea’. Preprint. PsyArXiv, 30 August 2020. https://doi.org/10.31234/osf.io/s7qj8.
Tags
- nationwide lockdown
- psychological outcome
- depression
- social factors
- public health
- loneliness
- mental health
- social distancing
- psychosis-risk
- general population
- physical health
- South Korea
- lang:en
- COVID-19
- demographic
- crisis
- behavioural science
- stress
- social network
- females
- anxiety
- is:preprint
Annotators
URL
-
-
www.irishtimes.com www.irishtimes.com
-
Taylor, Charlie. ‘Ireland Ranked among Best for Covid-19 Innovative Solutions’. The Irish Times. Accessed 7 September 2020. https://www.irishtimes.com/business/innovation/ireland-ranked-among-best-for-covid-19-innovative-solutions-1.4233471.
-
-
www.scientificamerican.com www.scientificamerican.com
-
Stix, G. (n.d.). Zoom Psychiatrists Prep for COVID-19’s Endless Ride. Scientific American. Retrieved June 9, 2020, from https://www.scientificamerican.com/article/zoom-psychiatrists-prep-for-covid-19s-endless-ride1/
-
-
www.ezekielemanuel.com www.ezekielemanuel.com
-
COVID-19 Activity Risk Levels. (n.d.). Ezekiel Emanuel | COVID-19 Activity Risk Levels. Retrieved July 8, 2020, from http://www.ezekielemanuel.com/writing/all-articles/2020/06/30/covid-19-activity-risk-levels
-
-
papers.ssrn.com papers.ssrn.com
-
Benvenisti, E. (2020). The WHO – Destined to Fail?: Political Cooperation and the COVID-19 Pandemic (SSRN Scholarly Paper ID 3638948). Social Science Research Network. https://papers.ssrn.com/abstract=3638948
-
-
www.forbes.com www.forbes.com
-
Perez, M. (n.d.). 55% Of U.S. Coronavirus Cases In CDC Analysis Are Black And Hispanic. Forbes. Retrieved June 28, 2020, from https://www.forbes.com/sites/mattperez/2020/06/15/55-of-us-coronavirus-cases-in-cdc-analysis-are-black-and-hispanic/
-
-
www.azdhs.gov www.azdhs.gov
Tags
- resource allocation
- healthcare
- lang:en
- COVID-19
- grouping
- priority
- care facility
- treatment
- public health
- is:pdf
- addendum
- scoring
- triage
- scarcity
Annotators
URL
-
www.reddit.com www.reddit.com
-
u/nick_chater (2020) Behavioural Policy Challenge: when does compulsion help? reddit. Retrieved from: https://www.reddit.com/r/BehSciAsk/comments/hzci8g/behavioural_policy_challenge_when_does_compulsion/
-
-
psyarxiv.com psyarxiv.com
-
Van Bavel, J. J., & Myer, A. (2020). National identity predicts public health support during a global pandemic [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/ydt95
-
-
-
Mathew, M. (2020). Lockdown stress amid COVID-19 on Alcoholics and Drug addicts [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/an8m4
-
-
jamanetwork.com jamanetwork.com
-
Luo, Z., Li, S., Li, N., Li, Y., Zhang, Y., Cao, Z., & Ma, Y. (2020). Assessment of Pediatric Outpatient Visits for Notifiable Infectious Diseases in a University Hospital in Beijing During COVID-19. JAMA Network Open, 3(8), e2019224–e2019224. https://doi.org/10.1001/jamanetworkopen.2020.19224
-
-
www.ajpmonline.org www.ajpmonline.org
-
Liu, Y., Finch, B. K., Brenneke, S. G., Thomas, K., & Le, P. D. (2020). Perceived Discrimination and Mental Distress Amid the COVID-19 Pandemic: Evidence From the Understanding America Study. American Journal of Preventive Medicine, 0(0). https://doi.org/10.1016/j.amepre.2020.06.007
-
-
www.healthline.com www.healthline.com
-
Blood Thinners, Blood Pressure Meds May Improve COVID-19 Survival Rate. (2020, August 27). Healthline. https://www.healthline.com/health-news/blood-thinners-blood-pressure-meds-may-improve-covid-19-survival-rate
-
-
www.nytimes.com www.nytimes.com
-
The New York Times (2020) C.D.C. Halts Evictions, Citing Covid-19 Risks. Retrieved from: https://www.nytimes.com/2020/09/01/world/covid-19-coronavirus.html?action=click&module=Top%20Stories&pgtype=Homepage#link-26bc7ab3
-
-
psyarxiv.com psyarxiv.com
-
Scott, S., Rivera, K., Rushing, E., Manczak, E., Rozek, C. S., & Doom, J. (2020). “I hate this”: A qualitative analysis of adolescents’ self-reported challenges during the COVID-19 pandemic [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/4ctb7
-
-
stresscontrol.ie stresscontrol.ie
-
Home. (n.d.). Stress Control. Retrieved September 2, 2020, from https://stresscontrol.ie/
-
-
www.scientificamerican.com www.scientificamerican.com
-
Barber, C. (n.d.). COVID-19 Can Wreck Your Heart, Even if You Haven’t Had Any Symptoms. Scientific American. Retrieved September 1, 2020, from https://www.scientificamerican.com/article/covid-19-can-wreck-your-heart-even-if-you-havent-had-any-symptoms/
-
- Aug 2020
-
-
Zhou, T., Nguyen, T. T., Zhong, J., & Liu, J. (2020). A COVID-19 descriptive study of life after lockdown in Wuhan, China [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/ygae5
-
-
www.thelancet.com www.thelancet.com
-
Chaudhry, R., Dranitsaris, G., Mubashir, T., Bartoszko, J., & Riazi, S. (2020). A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine, 0(0). https://doi.org/10.1016/j.eclinm.2020.100464
-
-
www.nature.com www.nature.com
-
Zheng, Q., Jones, F. K., Leavitt, S. V., Ung, L., Labrique, A. B., Peters, D. H., Lee, E. C., & Azman, A. S. (2020). HIT-COVID, a global database tracking public health interventions to COVID-19. Scientific Data, 7(1), 286. https://doi.org/10.1038/s41597-020-00610-2
-